3 Chapter 4 – An Exploration of Ultrasound Education and the Impact of Covid
Ultrasound Simulation: Friend or Foe?
haas483 and cadieux7
This chapter explores the impact of Covid on sonography education. Specifically, this chapter focuses on the historical methods of sonography education regarding scanning skills compared to the adapted instructional methods due to the Covid pandemic. Many ultrasound programs had to move their teaching to fully or partially remote because of Covid, including formerly in-person clinical rotations and educational practice labs. We used literature that researched ultrasound scanning training methods and we conducted recent interviews to provide up-to-date information regarding training during Covid. The gathered informational analysis will try to determine, “How has the increasing use of ultrasound simulations in ultrasound education impacted the scanning ability of students during the Covid pandemic?

Image of a current ultrasound scanning machine and transducer, obtained from Siemens Medical
A Historical Look at Medical Ultrasound Education
Diagnostic medical sonography is a field of medicine that utilizes imaging equipment and soundwaves to record and image different parts of the body. Ultrasound is non-invasive and can be used on almost any area of the body and helps detect and treat various medical conditions. Sonography is another term for ultrasound and the profession of a diagnostic medical sonographer is a trained medical professional who acquires ultrasound images. “Ultrasound is currently the second-most used clinical imaging modality after conventional X-ray radiography. Although ultrasound is considered to be a mature technology, technical advances are constantly being made” (Shung, 2011). This section will explore how medical ultrasound education has evolved over time, including changes in ultrasound equipment and the process of learning and using that equipment over time.
Early Years (On-the-job training)
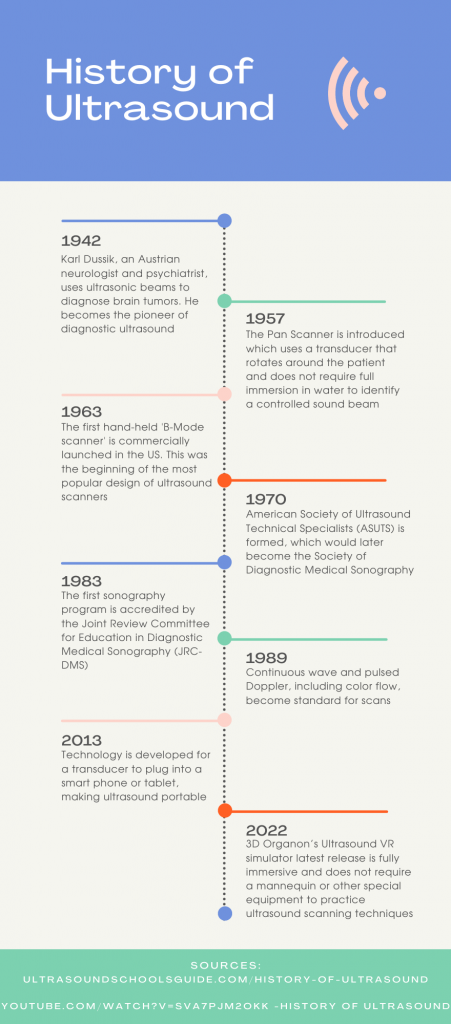
This portion will provide a look into the early years of ultrasound education prior to accredited sonography programs. In 1955 a Japanese physicist named Shigeo Satomura and his team implemented Doppler shift techniques in monitoring the pulsations of a heart and peripheral blood vessels. This was the first medical application of the Doppler Effect. Two years later in 1957, the Pan Scanner was introduced which did not require patients to be submerged underwater to obtain images and used a transducer that rotated around the patient to gain internal images of anatomy.

Image of an engineer submerged in a water bath to obtain ultrasound images, obtained from National Museum of American History
In 1963 the B-Mode scanner became available in the United States, which was the first hand-held scanner and one of the most popular designs of ultrasound scanners. Following this new technology, in 1965 Walter Krause and Richard Soldner invented a real-time imaging scanner, which offered the ability to scan and analyze ultrasound images immediately. In 1970 the American Society of Ultrasound Technical Specialists (ASUTS) was formed which would later become the Society of Diagnostic Medical Sonographers and then finally the Society of Diagnostic Medical Sonography (SDMS). The 1970s are when image quality began to be improved and color was able to be added and superimposed on 2D anatomical images (Ultrasound School Guide).

Ultrasound image of the liver displaying different gradations of grayscale and color, obtained from Zander, et. al
As technology developed, so did the job descriptions and opportunities associated with medical ultrasound. A sonographer must be able to capture and read images before moving on to the next set of images all before the physician has a chance to look at anything. There is a close relationship between the physician and the sonographer, and communication is very important. On-the-job training was the only way to become a sonographer before accredited programs and consisted of learning didactic information along with a scanning apprenticeship. Opportunities for specializing in different areas of the body became more prevalent and formal certificate programs were created as an option for those who wanted to specialize and typically already had ultrasound experience. Eventually, associate’s and bachelor’s degree programs were developed with a combination of lectures and clinical hours. The need for an organized definition of the occupation and the correlating educational criteria became apparent (Taylor-Fujikawa, et. al, 2019).
Image of a cardiac ultrasound with color overlay, obtained from SDMS website video
80s and 90s (First accredited sonography programs)
As technology has advanced, the education requirements have evolved as well. The first sonography program was accredited by the Joint Review Committee for Education in Diagnostic Medical Sonography (JRC-DMS) in 1983. This helped to standardize requirements and qualifications for graduating students who would be working professionally in hospitals and clinics. The National Education Curriculum includes requirements for anatomy and physiology, pathophysiology, mathematics, physics, communication skills, psychology and human behavior, informational technology, medical ethics and law, patient care, and ergonomics of proper scanning techniques to protect the health of sonographers. On-the-job training still existed, but graduates from accredited sonography programs gained popularity in medical environments like hospitals for billing purposes.
The time spent in school instead of on-the-job training made it difficult for some students, but hospitals began to see the benefits of hiring graduates who completed the rigorous set of standards determined by accreditation. The option to specialize in certain areas also became popular for areas including the abdomen and superficial structures, breast, musculoskeletal, OB-GYN, cardiac, pediatrics, and vascular technology. The following video gives a simplified timeline of the progression of ultrasound technology and education along with photos of how ultrasound imaging has improved from 1973 to present.
https://youtube.com/watch?v=sVa7PJm2okk
Video Credit: SDMS
Into the 2000s (Advances in Technology, more schools)
Presently, the Commission on Accreditation of Allied Health Educational Programs (CAAHEP) was created to ensure oversight and due process to all programs participating in its system of accreditation. Sonography students can earn a diploma, certificate, associate degree, bachelor’s or master’s degree before taking a certification exam. In 2019 there were 221 local universities, colleges, and schools in the United States that offer CAAHEP accredited ultrasound programs.
As educational and clinical opportunities have increased, the need for a certification exam arose to determine if graduates possess the necessary skills and confidence to become successful medical sonographers. “The benefits of certification include demonstration of knowledge, skills, and abilities through educational achievement; validation of clinical experience to prospective employers; and a clear, competitive edge over non-certified candidates” (Taylor-Fujikawa, et. al, 2019). Two of the certifying agencies include the American Registry of Diagnostic Medical Sonography (ARDMS) and the American Registry of Radiologic Technologists (ARRT).
In terms of prerequisites to enroll in a program and educational curriculum, the CAAHEP defines the following:
Prerequisites for one-year program:
- Applicants must possess qualifications in a clinically related allied health profession.
Prerequisites for two-year program:
- Applicants must be high school graduates (or equivalent) with an educational background in basic science, general physics, and algebra.
- All applicants must demonstrate satisfactory completion of the following courses at college level: general physics, biological science, algebra, and communication skills.
- Skills potential and practicing sonographers should exhibit include social perceptiveness, learning strategies, critical thinking skills, instructional skills, active listening, active learning, reading comprehension, and written/oral expression.
Curriculum:
- Physical sciences, applied biological sciences, patient care, clinical medicine, applications of ultrasound, instrumentation, related diagnostic procedure, and image evaluation.
A key component of an accredited program is well-structured, competency-based clinical education for students to experience clinical care in real-time (CAAHEP). During a student’s clinical rotation, it is possible for them to practice their ultrasound skills on mock patients, real patients, or utilize simulation technology to mimic real patients.
The following timeline briefly summarizes some of these important dates:
An Overview of Simulation Types for Sonography
There are three general types of simulation that can be used in sonography scanning education, starting with no simulation where a student is learning to scan on real patients in real-time, a second type called mock patient simulation where either volunteers or other students are utilized to practice and develop scanning skills, and finally virtual simulations which can include computers, virtual reality, or phone simulators. There are benefits and drawbacks to each type of simulation for sonography students who are learning and practicing their skills.
No simulation (learning on real patients)
When clinical education was first being developed, it was very common for students to learn scanning techniques and practice skills on real patients while providing a diagnostic examination. One of the schools we interviewed, School 4, used this method for years. They received their initial accreditation in the late 80s. Over time they implemented a one-week book camp that students attended prior to starting their clinical rotation. During the interview, the program director stated, “we eventually added a pre-clinical scanning course to teach basic scanning skills to students prior to starting clinical.” There are numerous benefits and disadvantages of this method outlined below:
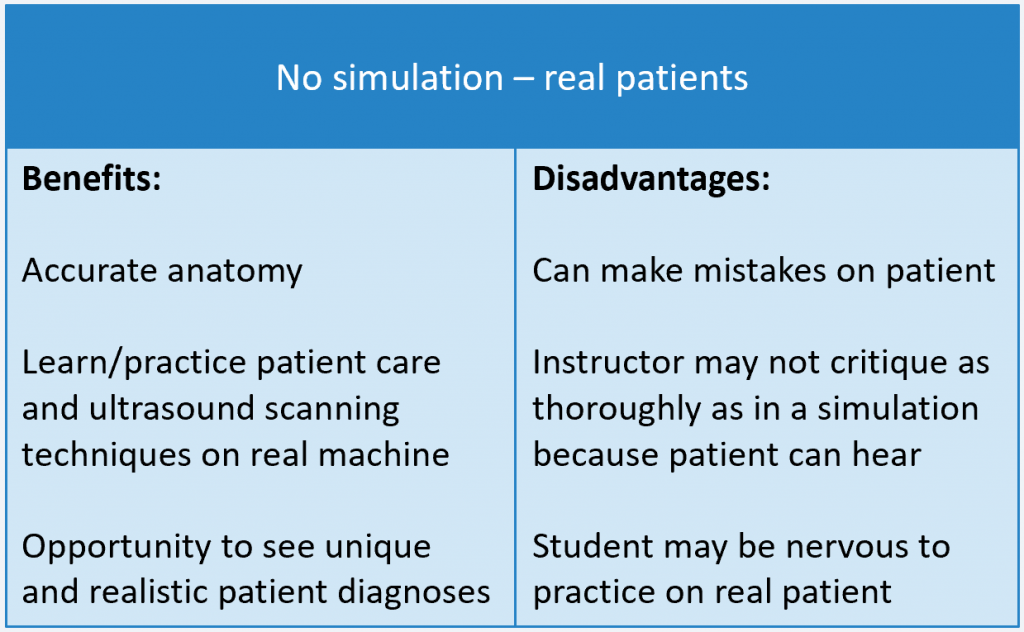
Sources: Shung, et al, Taylor-Fujikawa, et al
Mock Patient simulation
As clinical instructors revised and improved student clinical education, using mock patient simulation became more popular for many reasons. Mock patients are typically volunteers or other students in the sonography program who are available for students to practice and help develop their skills. Students are still practicing on real patients with real anatomy, but in a less stressful environment because these are not real patients undergoing diagnostic exams. This is the primary method of training within the four schools that we interviewed prior to Covid. The benefits and disadvantages of simulating with mock patients are outlined below:
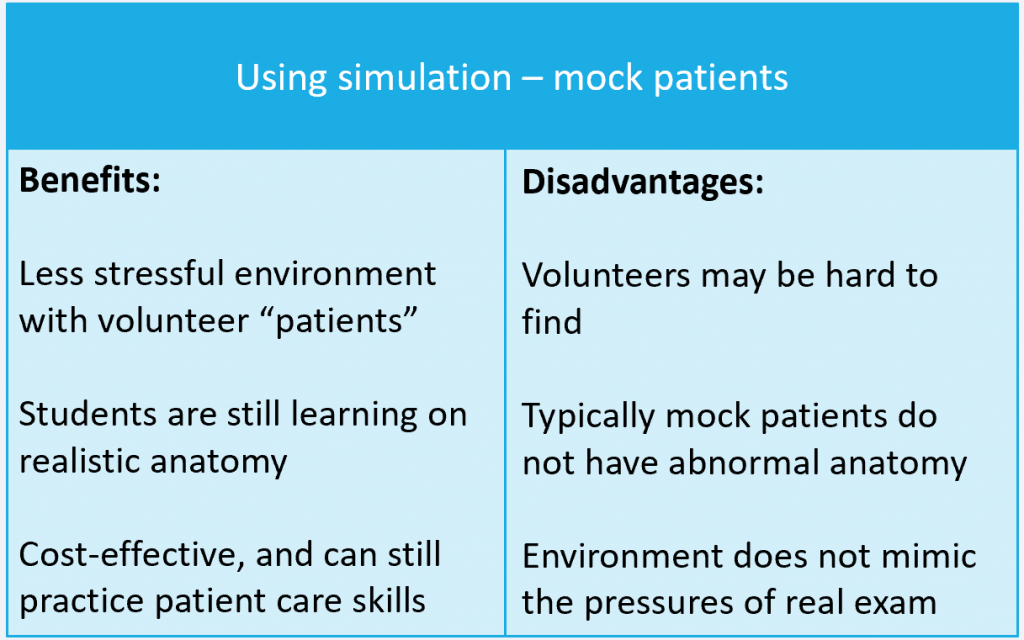
Sources: Zavitz, et al, Situ-LaCasse, et al
Computer, VR, Phone simulation systems
Advances in technology have enabled the use of computer simulations to take the place of real or mock patients in certain situations. Virtual reality is another form of simulation that is growing in popularity, and portable scanning using a probe attached to a phone is also being demonstrated. The following video is an example of a virtual reality simulator for education:
Video credit: 3D Organon
When access to real human anatomy is not possible, the option to develop and practice skills using these technologies can be valuable. However, solely relying on computer simulations without supplementing scanning on real or mock patients is unrealistic and puts students at a disadvantage. The benefits and disadvantages of simulating with computers, virtual reality, or phones are outlined below:
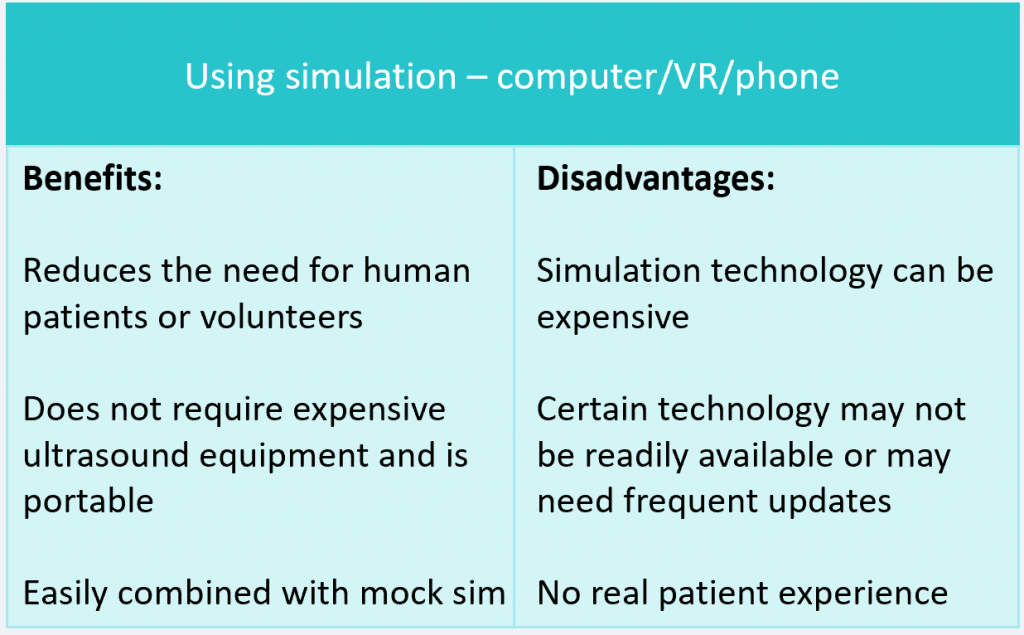
Sources: Bentley, et al, Merz, et al, Meuwly, et al, Zavitz, et al
Use of Simulation in Medical Ultrasound Education
This section explores the history of simulation use in sonography programs along with the changes due to Covid. “Ultrasound training varies greatly across training environments, programs, and specialties,” (Bentley, et al, 2015). Historically, multiple types of simulation have been used within sonography programs. Some changes to this practice were made due to Covid, where little or no contact was allowed. Schools reopened their class labs before clinical sites reopened for students, delaying clinical training. The use of technology in ultrasound simulation has improved over the years, with many new considerations of how to accurately teach anatomy and ultrasound scanning skills during Covid when many clinical sites had to switch to remote learning.
Pre-Covid
Here is a look at pre-Covid use of simulation and preferred methods of teaching scanning to sonography students when clinical rotations and labs were in-person. Sonography programs offer different learning opportunities when it comes to scanning training. Out of the four schools we interviewed, the typical simulation used pre-Covid was mock patients either scanning volunteers or other sonography students. Schools 1 and 4, used some computer simulation prior to Covid in conjunction with mock patients. Scanning volunteers is cost-effective and mimicked real patient obstacles, such as bowel gas and body habitus. Part of learning to scan is being able to develop critical thinking, cognitive, and motor skills when these obstacles occur (Bradley, K., Quinton, A., & Aziz, A., 2020). Lab training is followed by clinical rotations incorporating real patient scanning. Certain programs teach their scanning portion on real patients at clinical without simulation, this was an issue when clinical sites were closed to students during the onset of the Covid pandemic. Medical students In Switzerland attended an in-person training workshop prior to Covid and the lockdown prevented medical schools from conducting this workshop (Meuwly, et al, 2021). An online simulator was implemented for medical students to practice ultrasound on a virtual simulator (Meuwly, et al, 2021). Other programs already used computerized simulation systems before Covid. The scanning ability, limitations, and benefits will be analyzed more closely in the upcoming sections.

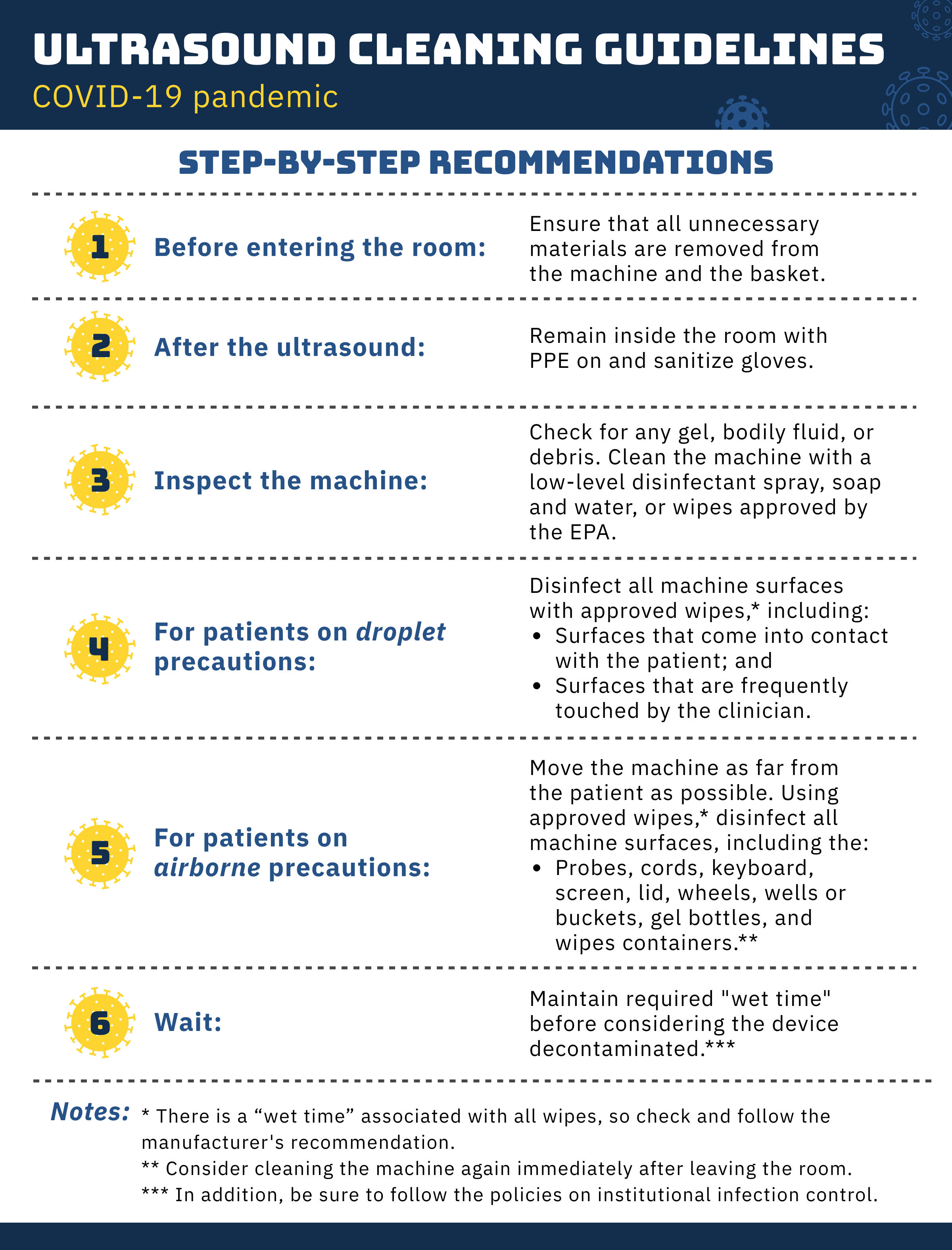
During Covid
“On March 17, 2020, the Association of American Medical Colleges recommended the temporary suspension of medical student clinical rotations,” (Gomez, et al, 2020). The shutdown was to ensure the safety of students and patients, allowing conservation of personal protective equipment (PPE) and maintaining social distancing. During the initial shutdown, schools closed for on-campus learning. Some sonography programs postponed the learning process until in-person learning could resume. Other schools adapted their teaching methods using online instruction and simulation.
In order to provide recent data regarding educational adjustments during Covid, we interviewed four CAAHEP accredited sonography programs in Texas. School 1 stated they used some computer simulation prior to Covid, but did not divulge which brand they used. They provided didactic learning during the shutdown and modified their lab training once the students returned to campus. They split their labs to lower the amount of contact with fewer students while providing “real person” scanning and computer simulation. School 3 used Simtics for sonography and stated Simtics was only used during the short duration when campuses were closed, and that the school resumed mock patient scanning afterward with safety modifications.
Example of Simtics Scanning Video
Simtics Ultrasound Training Liver Video
School 3 continued with online instruction and used some of this time to supplement the student’s clinical hours by critiquing sonography images and watching YouTube videos of common and rare scans that are not likely to be seen otherwise. This was followed by a discussion and reflection regarding the video training. This was only used for a short duration that was approved by the accrediting bodies. School 2 used SonoSim online until they were able to return to full face-to-face classes and labs in July 2020. School 4 changed its scheduling to do didactics one day and labs on separate days since the lecture was virtual. They used clear shower curtains with cut holes to practice scanning on volunteers. This was used to create a barrier between the student and scanning volunteer until the end of 2020.

They acquired additional scanning phantoms to use in the lab during Covid, to minimize student exposure and because no volunteers were allowed in the lab. All schools with computer simulators have continued to use them on campus in conjunction with mock patient scanning. They also purchased Butterfly transducers, that were issued to students who had to quarantine at home. The Butterfly transducer is used with mobile devices and tablets. This device allows a person to scan as if they had a personal ultrasound system. School 1 and school 2 did not modify their clinical hours, they resumed once the sites allowed students to return.

When reviewing the literature, other universities also used alternative methods for remote learning during the shutdown. The literature covered multiple medical fields, including sonography. One university used prerecorded lectures and remote didactics via Zoom, interactive remote workshops, case sessions, online quizzes, and jeopardy sessions (Gomez, et al, 2020, p 1286). Another article was specific for ultrasound students regarding teaching them basic psychomotor skills during the shutdown (Meuwly, et al, 2021). The students practiced ultrasound exercises on a virtual simulator, using a mouse as a simulated ultrasound probe. This is a similar experience to the school that used Simtics. Another medical school had their students watch live scanning demonstrations remotely and practiced using a cellular phone to simulate probe movement (Zavitz, et al, 2021). In Singapore, radiology residents used self-ultrasound to maintain ultrasound training, like other departments they used webinars and video platforms for teaching purposes (Tang, et al, 2020). The self-ultrasound helped minimize human interaction during the shutdown.

Analysis of Sonography Scanning Ability
After compiling research article information and conducting interviews with sonography program directors, we reviewed different simulation types, an analysis of scanning ability is provided within this section.
No simulation (Learning on real patients.)
Traditionally, many sonographers learned their skills on real patients in clinical practice. This includes some current sonography programs as well as cross-training from other imaging modalities. With the increase in patient load, the clinical site preceptors have less time to teach the basic scanning skills needed for optimizing system settings, proper ergonomic scanning techniques, and scanning protocols (images required for specific studies). Most sonography programs today utilize some type of simulation prior to clinical rotations. This allows the clinical site instructor to spend time with the student on fine-tuning skills, rather than basic skills.
Mock patient simulation
In Australia, a four-year undergraduate-postgraduate course introduced ultrasound simulation using peers as standardized patients (Bowman, et al, 2020). As with many institutions, this is a cost-effective way to teach sonography students how to navigate the real-life obstacles that occur with scanning patients. The Australian study showed transfer of skill improved with simulation in conjunction with increased deliberate practice and feedback (Bowman, et al, 2020). Scanning peers and self-ultrasound offers limited exposure to significant pathology; however, it is thought that recognizing normal over an abnormal appearance will be more obvious. Of course, the pathology may need to be identified but the most crucial factor is that pathology is not missed during the ultrasound examination.
The advantages of mock patients or self-ultrasound over a computer simulator experience are building the skills for working around bowel gas, breath holds, full bladders, and nil per os (NPO) status. This practice creates an empathetic response with patients and being able to adjust the probe with different appropriate amounts of pressure is something difficult to correlate with a computer simulator and real patients. One potential limitation to demonstrating a scan on a mock patient in the ultrasound lab is every student in the lab tends to crowd around one station to watch (Loria, K., Ultrasound News: Reimagining the Sonography Lab). This can make it difficult for students to view all the steps during the demonstration.
Computer simulation
Multiple studies have been conducted to assess scanning ability with the use of computer simulation. Most of the studies conducted assessed simulation in teaching the focused assessment with sonography for trauma (FAST) exam which is a life-saving tool in the emergency department (Bentley, et al, 2015). The FAST exam uses ultrasound but is different from performing a full diagnostic ultrasound examination. It is thought that using a computer simulation streamlines the education process by reducing the need for ultrasound machines and human models for scanning (Bentley, et al, 2015). Bentley and associates also suggest that a notable advantage of simulation is exposure to both normal and pathological examinations increasing proficiency and skill level (2015). The limitations of this study include using small sample size and the medical students demonstrating the FAST exam; however, the study revealed simulation was non-inferior to traditional methods used in ultrasound education (Bentley, et al, 2015). Another study by Situ-LaCasse and associates suggests novice medical students can learn basic skills in image acquisition by reviewing online modules using SonoSim (2021). Again, this is a study used for a point-of-care ultrasound which is like the FAST exam. “The main criticism rests on the scarcity of scientific studies analyzing the real impact of simulation-based ultrasound training on clinical practice,” (Meuwly, et al, 2021).
In our interview process, School 1 stated, “computer simulation cannot represent a real patient no matter how expensive or new it is.” School 2 was asked if students showed improvement in scan ability after implementing SonoSim. They stated, “very limited and is not justified by cost, but will consider using it to augment scan training.” Schools that were interviewed reported they will be using computer simulators in conjunction with scanning mock patients moving forward.
Example of FAST exam tutorial.
Video Credit: Radiology Nation
The Future of Sonography Training
This section will provide an overview of learning sonography scanning skills over time and the implications of the future in sonography training based on analysis. This will explore the impact of simulation and its changes in how sonography is taught.
Benefits of simulation
The benefits of mock patient simulation include using live subjects that will provide a realistic experience while scanning. Computer simulation provides an opportunity to view normal and abnormal findings during the duration of the scan experience. “The ultrasound simulator allows a fairly realistic assessment of pathological findings,” (Merz, 2006). Even in the clinical setting, some pathologies are rarely seen. Computer simulation will allow the student to practice alone and not require someone else to scan; however, self-ultrasound is an option as indicated by Tang in the letter to the editor on “Maintaining Training with Self-Ultrasound During Covid-19.” Regarding student scanning ability, there are some benefits to simulation, especially for novice students as seen in the FAST scan studies and feedback from our interviews. Another benefit is remote learning which could become prevalent again in the future or could be utilized in rare circumstances if a student is unable to attend in-person clinical for a period.
Limitations of simulation
The limitations of mock patient scanning simulation include scanning the same individuals repeatedly which allows the student to learn that person’s anatomy and abnormal findings. Real patients are the great unknown, so the ability to find pathology is crucial; there is a comfort level established by scanning the same people. Computer simulation is not realistic for gauging the amount of pressure to apply on patients, or breath holds for patients and prepping the patient for the exam. Computer simulations provide a range of capabilities, some provide stickers on the mannequin for probe placement. The sonographer must move the probe to find the best scanning window and this simulator is limited in that aspect. Other limitations include image quality and case selections with certain simulators. The need for improvement in simulation to provide a better learning experience in scanning ability includes these factors for making it more realistic for the advanced student. Manipulation of the probe is micro and macro movements are part of the skill acquired while scanning, simulators do not provide that type of feedback. Merz states, “a dummy only partly reflects the experience of examining a real patient,” (2006). Both mock patient and computer simulators incur expenses whether it is ultrasound machines or computer simulators, this is a moot point.
Benefits and Limitations of Simulators
| Benefits | Limitations |
|---|---|
| Doesn’t require a body to scan | Doesn’t require altering probe pressure |
| Demonstrates normal and abnormal findings | Using alternate windows can’t be practiced |
| Allows remote learning | No real patient dynamics (breath hold etc,.) |
| Doesn’t require patient prep (full bladder, NPO) | Limited sections without definite landmarks for orientation |
| Improve the diagnostic rate of common abnormalities | Some don’t show moving objects (fetal heart, Doppler) |
| Limited image quality | |
| Some don’t allow system adjustments (gain, TGC) |
Conclusion
In summary, the advances in technology from the early days of ultrasound to the more advanced equipment used today, have impacted how sonography has been taught through time. The Covid-19 pandemic created an opportunity for many schools to rethink their methods of teaching sonography. The sonography programs we interviewed seem to have adjusted through the pandemic and continue to incorporate some type of computer simulation in their training on an ongoing basis. All the schools interviewed stated that nothing replaces the experience of scanning a real person. Each computer simulation has limitations but can provide some benefits to use in conjunction with mock patient simulation.
How has the increasing use of ultrasound simulations in ultrasound education impacted the scanning ability of students during the Covid pandemic? In studies we reviewed and in schools that were interviewed, simulation improved scanning ability with students that scanned mock patients in conjunction with computer simulation for full diagnostic ultrasound examinations. Within the studies that explored training for FAST exams, simulation provides adequate training for the quick study needed in emergent cases. “Simulation however cannot replace traditional training methods entirely, and further research is needed to assess how to effectively incorporate simulation into ultrasound education, (Bradley, K., Quinton, A., & Aziz, A., 2020).
References
Bentley, S., Mudan, G., Strother, C., & Wong, N. (2015). Are Live Ultrasound Models Replaceable? Traditional versus Simulated Education Module for FAST Exam. The western journal of emergency medicine, 16(6), 818–822. https://doi.org/10.5811/westjem.2015.9.27276
Bowman, A., Reid, D., Bobby Harreveld, R., & Lawson, C. (2021). Evaluation of students’ clinical performance post-simulation training. Radiography, 27(2), 404–413. https://doi.org/10.1016/j.radi.2020.10.002
Bradley, K., Quinton, A., & Aziz, A. (2020). Determining if simulation is effective for training in ultrasound: A narrative review. Sonography, 7(1), 22–32.
Commission on Accreditation of Allied Health Education Programs, retrieved from https://www.caahep.org/Students/Program-Info/Diagnostic-Medical-Sonography.aspx
Gomez, E., Azadi, J., Magid D. (2020). Innovation Born in Isolation: Rapid Transformation of an In-Person Medical Student Radiology Elective to a Remote Learning Experience During the COVID-19 Pandemic, Academic Radiology. Science Direct 27(9), 1285-1290. doi:10.1016/j.acra.2020.06.001
Loria, K. (n.d.). Ultrasound News: Reimagining the Sonography Lab. Retrieved March 10, 2022, from https://www.radiologytoday.net/archive/rt0321p26.shtml
Merz, E. (2006, September). (PDF) ultrasound simulator – an ideal supplemental tool … ResearchGate. Retrieved April 1, 2022, from https://www.researchgate.net/publication/6861497_Ultrasound_simulator_-_an_ideal_supplemental_tool_for_mastering_the_diagnostics_of_fetal_malformations_or_an_illusion
Meuwly J., Mandralis K., Tenisch E., Gullo G., Frossard P., Morend L. (2021). Use of an Online Ultrasound Simulator to Teach Basic Psychomotor Skills to Medical Students During the Initial COVID-19 Lockdown: Quality Control Study. JMIR Med Educ 7(4). doi: 10.2196/31132
Shung, K. K. (2011). Diagnostic ultrasound: Past, present, and future. J Med Biol Eng, 31(6), 371-4.
Situ-LaCasse, E., Acuña, J., Huynh, D., Amini, R., Irving, S., Samsel, K., Patanwala, A., Biffar, D., Adhikari, S. (2021). Can ultrasound novices develop image acquisition skills after reviewing online ultrasound modules? BMC Med Educ 21(175). doi/10.1186/s12909-021-02612-z
Tang, P., Chen, E., Liang, M., Teo, S., Ong, C. (2020, October 1). Maintaining training with self-ultrasound during COVID-19. Academic radiology. Retrieved March 10, 2022, from https://pubmed.ncbi.nlm.nih.gov/32800445/
Taylor-Fujikawa, J., Andrist, L. (2019, November 1). The (Updated) History of Sonography: Education and Credentialing. Journal of Diagnostic Medical Sonography. 35(6):520-524. doi:10.1177/8756479319876233
Zander, D., Hüske, S., Hoffmann, B., Cui, X. W., Dong, Y., Lim, A., Jenssen, C., Löwe, A., Koch, J., & Dietrich, C. F. (2020). Ultrasound Image Optimization (“Knobology”): B-Mode. Ultrasound international open, 6(1):14–24. doi:10.1055/a-1223-1134
Zavitz, J., Sarwal, A., Schoeneck, J., Glass, C., Hays, B., Shen, E., Bryant, C., Gupta, K. (2021). Virtual multispecialty point-of-care ultrasound rotation for fourth-year medical students during COVID-19: Innovative teaching techniques improve ultrasound knowledge and image interpretation. AEM Educ Train. (5). doi:10.1002/aet2.10632
