Chapter 15: Neurobiology of Trauma in Human Trafficking Survivors
Hannah R. Steinke, MSW, Social Work Doctoral Student, Contributing Author
ABSTRACT
The very nature of human trafficking evokes trauma. Traumatic experiences can result in significant alterations in brain structure and function, leading to widespread and long-lasting physical and psychological consequences. Social workers are often embedded at the intersection of systems, allowing the social worker to occupy a unique space from which to employ knowledge of the neurobiology of trauma in direct practice, policy, and research.
Learning objectives
By the end of this chapter, the student will be able to:
- Apply the biopsychosocial model to human trafficking
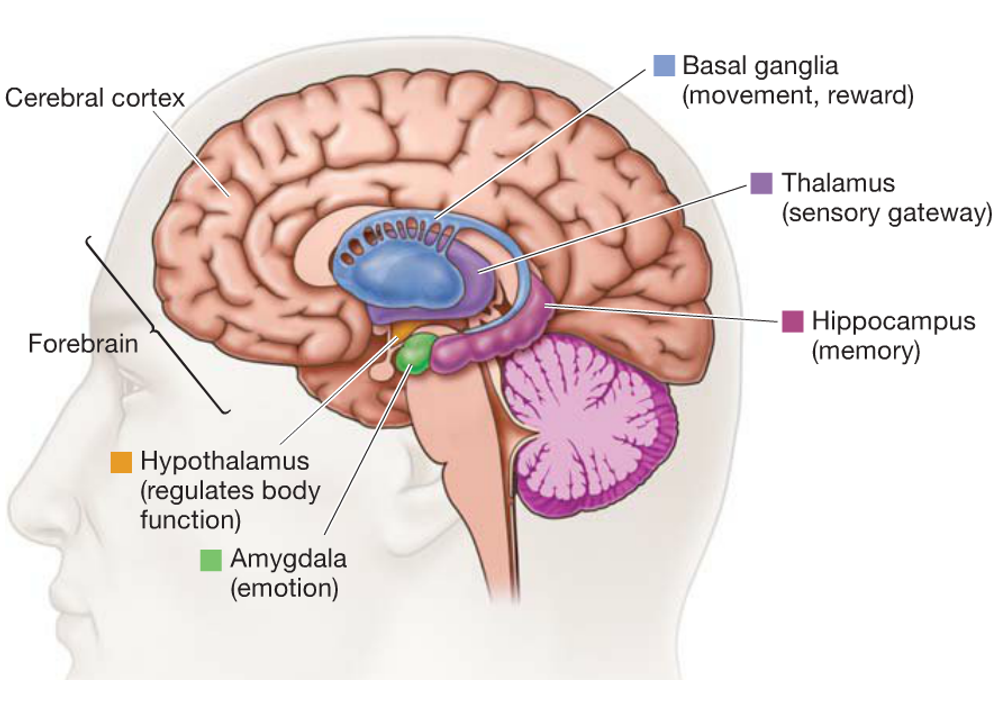
- Understand the role of the primary brain regions involved in stress response
- Apply constructs from neuroscience and the neurobiology of trauma to prevention and intervention efforts
Key Words: biopsychosocial model, stress response, HPA axis, neuroplasticity, acquired brain injury
GLOSSARY
Biopsychosocial model: a holistic framework that emphasizes the interconnectedness of the biological, psychological, and social facets of human functioning and experiences
Trauma: the physical or emotional response to a terrible event or set of circumstances
Stress: any force or demand exerted on the body that results in a change in the body’s homeostatic state (optimal state)
HPA axis: hypothalamic-pituitary-adrenal (HPA) axis – a chief regulatory neuroendocrine system responsible for widespread communication throughout the body
Neurotransmitters: are the chemical messengers found within the nervous system that transmit signals between nerve cells (neurons) or between neurons and other cells (e.g., muscle, glands).
Neuroplasticity: the brain’s ability to reorganize itself in response to experiences, learning, or injury
The Biopsychosocial Model
There are many perspectives, models, and theories that provide social workers with frameworks in which to ground their work with clients and larger systems. Among these perspectives is the biopsychosocial model – a holistic framework that emphasizes the interconnectedness of the biological, psychological, and social facets of human functioning and experiences (Figure 1). Though applied to social work practice, Engel’s biopsychosocial model emerged from the field of medicine as a rebuttal to the biomedical model – a model that narrowly focuses on the biological and medical factors of health and disease (Saraga et al., 2015). Engel argued that the social, psychological, behavioral, and biological aspects of health and disease are part of an integrated whole (Saraga et al., 2015). Further, Engel highlighted the role of culture and social factors in disease causation and treatment. The biopsychosocial model was among the first formal frameworks to recognize psychological responses to life (Engel, 1977, as cited in Saraga et al., 2015) as a critical factor in disease etiology (Saraga et al., 2015). Research supports that what happens at the relational level is directly related to the biological processes within the body – both in that biology can shape relationships and relationships can shape biology (Siegel et al., 2020).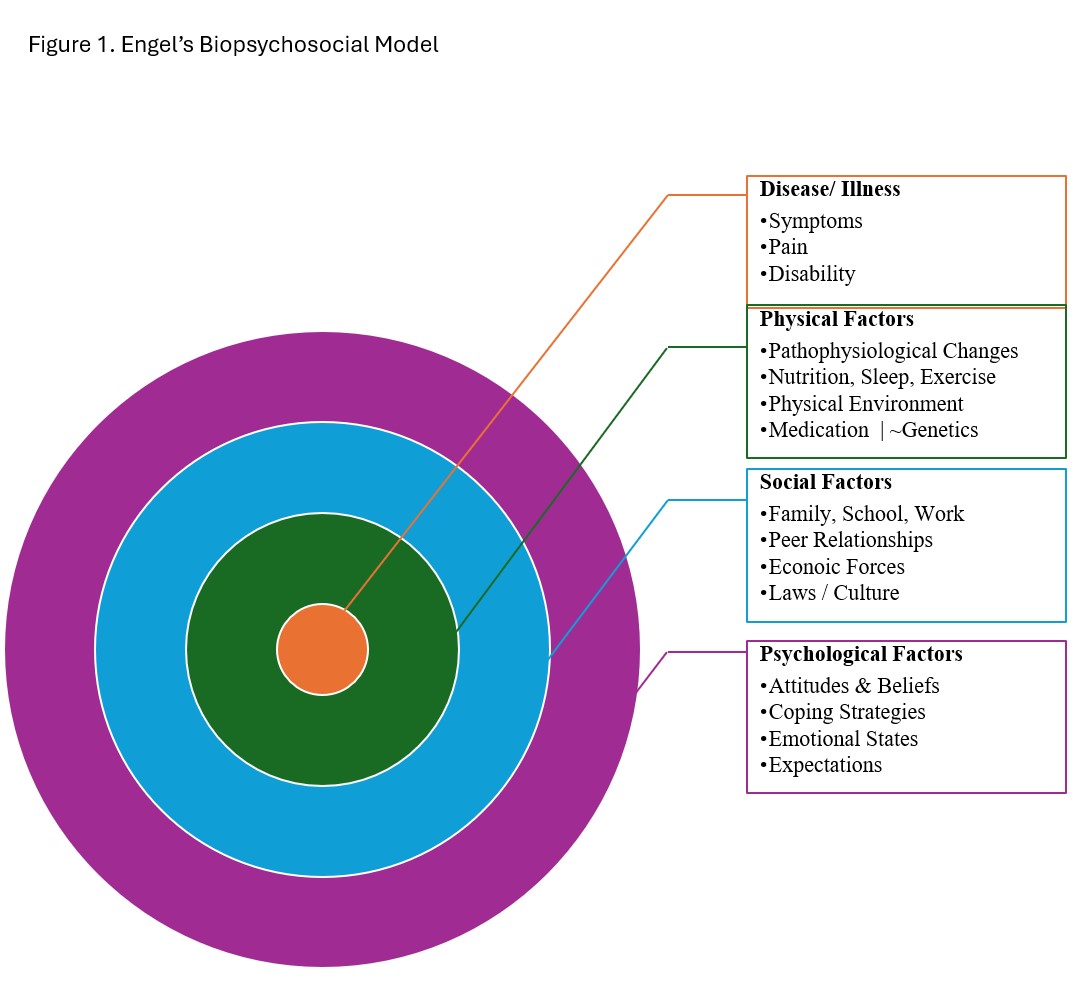
Though social work knowledge has been built upon constructs highlighting the importance of the social and physical environment, one could argue that the biological aspects of the biopsychosocial model are too often overlooked in social work practice. Moreover, few social workers acknowledge or fully understand the role the human brain plays in social justice issues plaguing society. However, because of its plasticity (ability to change), the human brain is integrally part of the bidirectional relationship between the social environment and the embodied experiences of every individual. Siegel (2012) describes the mind as “embodied in an internal physiological context and embedded in an external relational context” (p. xxv). In other words, the environment shapes the human brain, which in turn shapes the environment via individual and collective behaviors (Green & McDermott, 2010).
Why is it important for social workers to understand the neurobiology of trauma?
Social workers provide services at the intersection of many systems through direct practice, advocacy, activism, and policy development (among other diverse roles). As such, it is critical for social workers to possess well-rounded, interdisciplinary knowledge related to the social problems they seek to address. Green and McDermott (2010) argue that the mere relevance of social work practice rests in the discipline’s ability to gain and incorporate contextual knowledge of the environments in which social problems are embedded, including the biological environments. The authors add that to work successfully towards solutions to social problems informed by reductionist perspectives, social workers must integrate extant knowledge of the structure and function of the environments impacting such social issues. One powerful and important area of interdisciplinary knowledge is found within a niche space between the “hard” and “soft” sciences, with the incorporation of neuroscience into social work practice. Through knowledge of the brain and nervous system, social workers can better understand the dynamic interplay between an individual, the environment (Cozolino, 2024; Farmer, 2009; Green & McDermott, 2010; Matto et al., 2014), and the mechanisms and effects of trauma from both physical and nonphysical forms of violence (Wong et al., 2014). Within the context of human trafficking, a neurobiological perspective of trauma helps the social worker recognize how trauma responses are hard-wired to keep the trafficked person alive, even when these responses might seem counterintuitive.
Understanding Trauma
The word “trauma” has become part of everyday language for many Americans, but what is trauma? Interestingly, trauma is often defined as both an event and a reaction. The American Psychological Association (APA, 2025) defines trauma as the physical or emotional response to a terrible event or set of circumstances (e.g., crime, accident, death of a loved one, combat, natural disaster, abuse, neglect, experiencing/witnessing violence, etc.). Exposure to traumatic events can result in a wide array of profound biological, psychological, and social consequences. For survivors of human trafficking (as well as other vulnerable populations), the traumatic experiences endured are often numerous and extend across the lifespan. (*See an article on Adverse Childhood Experiences [ACEs] and Human Trafficking.]
Best practice recognizes trauma-informed care as a foundational facet of social work practice. Levenson (2017) discusses how all social workers (micro and macro) should be able to:
- Recognize factors/pathways that increase the likelihood of trauma symptomology.
- Know the signs and symptoms of trauma.
- Contextualize presenting concerns within a client’s history of traumatic experiences.
- Respond to trauma from a strengths-based perspective with respect, compassion, and empowerment, promoting client self-determination and agency.
- Adhere to the core values of social work to promote social justice by avoiding pathologizing behaviors and recognizing the complex intersections between multiecological factors that play a role in adversity across the lifespan.
A trauma-informed social worker will exemplify these principles in thought, language, and action. With this being said, language is perhaps one of the most powerful and foundational aspects of social work practice because language reflects thought and promotes action. For example, in the context of human trafficking, minimizing (e.g., downplaying their experience) or mutualizing (e.g., assigning equal blame/responsibility to the trafficked person and the trafficker) language can have detrimental effects, including increasing traumatic sequalae (secondary trauma) and preventing survivors from having access to much-needed services.
Stress and Traumatic Stress
To better understand trauma, it is helpful to understand stress and the stress response from a biomedical perspective (*see Kirby et al., 2024 for detailed definition and explanation of stress). While there are various definitions of stress, a simple way of thinking about and defining stress is: any force or demand exerted on the body that results in a change in the body’s homeostatic state (i.e., optimal set point; *see Kirby et al., 2024 for an in-depth description of homeostasis). From this perspective, we can broaden our view of stress to include both negative (e.g., bad, painful, fearful) and positive (e.g., good, pleasurable, exciting) stimuli (stressors), as well as both real (e.g., a violent act) and implied (e.g., threat of violence/thought about a past or potential violent act) (Muroy et al., 2024). Stress is one of the body’s central adaptive mechanisms because the purpose of stress is to promote survival by altering the body’s state and functioning to meet the demands placed on the body before returning the body to a state of homeostasis. Though stress can be beneficial, it can also become problematic when the stress response lasts too long, is too intense, or when the individual lacks the capacity to cope with the stressor. In clinical social work practice, we often see the effects of toxic stress (stress overload) in the form of post-traumatic stress disorder (PTSD), other mental and physical health issues, addiction, harsh parenting, etc.
Trauma, Brain Regions, and Neuroendocrine Communication
There are many very complex mechanisms contributing to the neurobiology of trauma, so much so that one could spend a lifetime learning these processes. However, three major brain regions play a significant role in response to stressors/traumatic stimuli/events – the amygdala, the hippocampus, and the prefrontal cortex. Additionally, one cannot discuss stress response and trauma without discussing the hypothalamic-pituitary-adrenal (HPA) axis – a chief regulatory neuroendocrine system responsible for widespread communication throughout the body (Leistner & Menke, 2020). The purpose of introducing these brain regions and their associated circuitry is to inform social workers of what is happening within the brain of the trafficked person, how this impacts the individual’s immediate functioning, and how these mechanisms affect treatment and recovery.
The amygdala is a small, almond-shaped structure deep within the temporal lobes of the brain. While the amygdala has many functions, it is often referred to as the “alarm center” of the brain because of its role in threat detection (particularly via processing negative emotions and fear) and initiation of the stress response systems (i.e., fight-or-flight). The amygdala plays critical roles in regulating fear conditioning, anxiety, aggression, social cognition, and emotional memory (AbuHasan et al., 2023). As with all neural structures, the amygdala does not function in isolation, but it is intricately and complexly connected to other brain regions through well-studied neural circuitry.
The hippocampus, a small seahorse-shaped structure located in the temporal lobe, is well known for its association with memory formation and spatial navigation, leading some to refer to this structure as the brain’s “flash drive” (Fogwe et al., 2023). Because of its functional roles in memory consolidation and emotional processing, the hippocampus is integrally involved in decision-making processes, including processing and storing verbal and symbolic information to be used for decisions related to future safety.
The prefrontal cortex is an area of the brain significantly impacted by trauma, including non-physical forms of interpersonal violence and coercive control. Some describe this area as the “personality center” of the brain. The prefrontal cortex is responsible for appraising situations, higher-level thinking, decision-making, impulse control, and emotional regulation (Hathaway & Newton, 2023). Particularly salient to the experiences of trafficking survivors is the fact that the prefrontal cortex enables an individual to adapt to situations, circumstances, and situational surroundings in decision-making and response to traffickers/abusers. This is a very important fact for social workers to understand because, many times, society judges the choices and behaviors of victims of human trafficking, intimate partner violence, and other relationships where coercive control is present. When we begin to understand how the brain works to keep an individual safe, we can begin to understand some of the survival mechanisms that influence human behavior.
The HPA axis plays a primary role in regulating the body’s stress response system. Not only does the HPA axis help the body adapt to stressors through “fight or flight” mechanisms, but it also works to maintain homeostasis by returning the body to a state of “rest and digest” after a threat is no longer detected. When a threatening cue is processed within the hippocampus and prefrontal cortex, a message is sent to the amygdala, the brain’s alarm system. The amygdala, in turn, mediates a neuroendocrine response via the sympathetic nervous system (SNS) and the HPA axis (Muroy et al., 2024). Within the HPA axis, the hypothalamus serves as the command center of the brain, communicating with the rest of the body and, in particular, with the autonomic nervous system (ANS) – a system comprised of two distinct but interrelated parts, the SNS and the parasympathetic nervous system (PNS). The SNS is often described as the “gas pedal” due to how it initiates the “fight or flight” response, while the PNS is often described as the brake system because of how it acts to restore the body to a state of “rest and digest”.
When a signal of distress reaches the hypothalamus, the hypothalamus releases increased amounts of corticotropin-releasing hormone (CRH), which in turn causes the pituitary gland to increase its production of adrenocorticotropic hormone (ACTH). When ACTH is secreted from the pituitary gland, it causes the adrenal cortex to synthesize and release glucocorticoids (GCs), such as cortisol (Leistner & Menke, 2020; Muroy et al., 2024). As the glucocorticoids circulate throughout the body, they suppress immune functions. Upon reaching the brain, the glucocorticoid receptors initiate a negative feedback loop, preventing the release of additional glucocorticoids and thus stopping the fight/flight response via the activation of the PNS (Muroy et al., 2024).
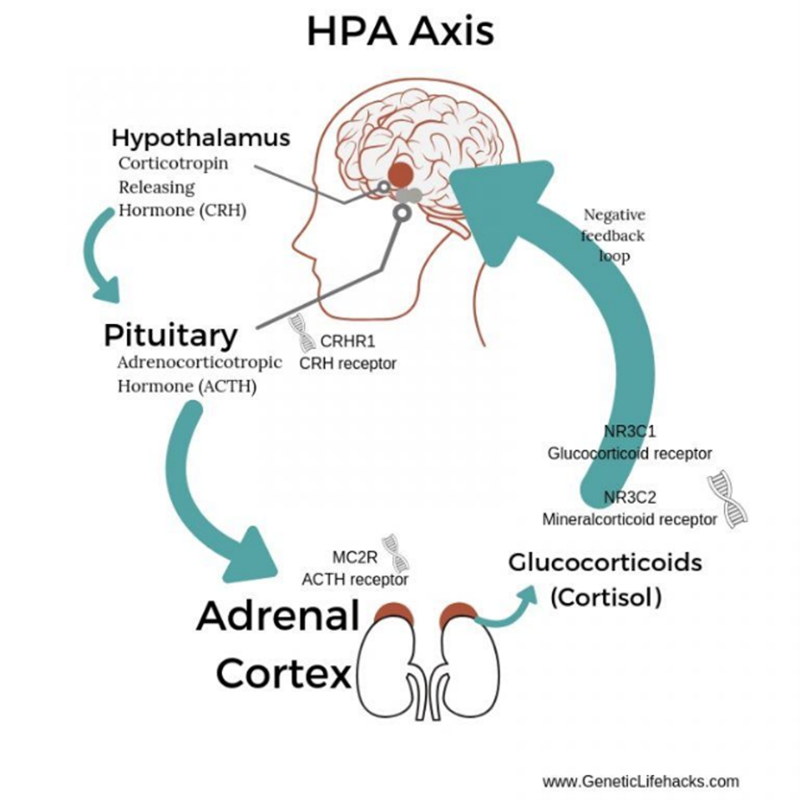
Although the tightly integrated stress response systems predictably react to stress, there is significant variability in stress responses and resilience between individuals. Among the factors affecting interindividual variability are genetic factors, early childhood stress, aging, sex-specific differences in molecular and biological functioning, and differences in perception and appraisal of situations (McEwen et al., 2015; Muroy et al., 2024). Conversely, factors promoting increased resilience are social support and social buffering, a sense of agency and personal control, meaning-making/purpose, and increasing compensatory mechanisms that decrease the allostatic load (McEwen et al., 2015).
Trafficking and Trauma
There are countless ways in which the trafficked person is impacted by their traumatic experiences. While this chapter does not allow for a deep exploration of the topic, four primary pathways will be briefly discussed: structural alterations, functional alterations, chemical (neurotransmitters) alterations, and neuroimmune response. These four effects provide the basis for understanding adverse childhood experiences (ACEs) and adverse health outcomes, as well as the host of physical and mental health disparities among survivors of human trafficking. Social workers must understand the implications of non-physical sources of trauma in addition to physical injuries. While trafficking survivors are known to experience horrendous physical injuries, the coercive control and non-physical assaults on their personhood are more likely to impact their long-term health than an isolated physical injury would. Further, the cumulative effect and duration of coercive control and violence play a significant role in outcomes for any individual experiencing chronic or long-term abuse.
The brain is unique in that it is highly sensitive to changes both internally (within the body) and externally (relationships, situations, and the physical environment). This sensitivity promotes neuroplasticity – the brain’s ability to reorganize itself in response to experiences, learning, or injury (e.g., growing new neural connections, killing off neural connections, and increasing the strength of existing connections). Traumatic experiences (both physical injury to the head and chronic/traumatic stress) can alter the structure and function of the brain. Trauma and stress-related structural alterations include some regions becoming more activated and potentially increasing in volume, while other structures shrink or decrease in volume. For example, research has noted reduced hippocampal volume, due to the effects of stress hormones, among individuals with histories of trauma (Logue et al., 2018). Studies also note increased activation and strengthening of connections within the amygdala among trauma survivors (promoting fear conditioning). Further, the threshold for activation can change as well as the appraisal of stimuli. This is classically evident in individuals experiencing hyperarousal and hypervigilance. Such increases in amygdala activity can make it difficult for an individual to recognize when a threat is no longer present (Bremner, 2006). During acute or prolonged stress, functional alterations occur as more primitive brain regions (e.g., amygdala and basal ganglia) take over for higher-order areas such as the prefrontal cortex. When this happens, individuals can experience difficulty with critical thinking, decision-making, cognition, and impulse control.
Brain chemistry can also be altered due to trauma, and in individuals where brain chemistry is already imbalanced, the impacts of traumatic events/stress can be more profound. Neurotransmitters are the chemical messengers found within the nervous system that transmit signals between nerve cells (neurons) or between neurons and other cells (e.g., muscle, glands). When neurotransmitter levels become imbalanced due to trauma/stress, various problems can arise, including (but not limited to) mental health symptoms/conditions (e.g., depression, anxiety, PTSD, mood swings, behavioral issues, risk-taking, propensity for addiction, etc.), cognitive issues (difficulty concentrating, brain fog, memory issues, attention difficulties, cognitive decline, etc.), and physical symptoms (e.g., sleep disturbances, chronic pain, digestive issues, appetite changes, etc.) (Bremner, 2006).
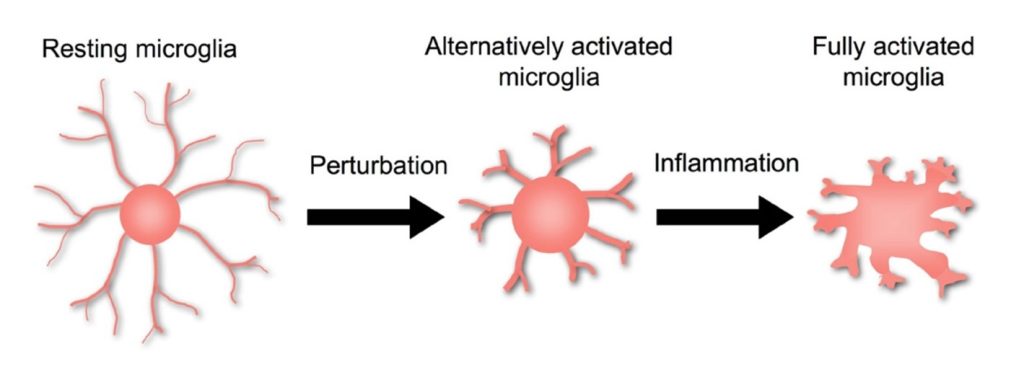
The neuroimmune system is very complex. However, what is important to note, in relation to trauma, is how impactful the neuroimmune system is on long-term mental and physical health outcomes. Chronic stress can alter immune function, particularly microglial cells, the primary immune cells of the brain. Glial cells (i.e., microglia, astrocytes, oligodendrocytes, ependymal cells) are dynamic cells, sensitive to changes within the environment. Microglia have two states: resting (homeostatic) and activated (reactive). During the resting state, microglia are far from inactive. Instead, microglia survey the environment within the central nervous system, ensuring a state of homeostasis is maintained. In this state, microglia are nurturing and supportive of neuron growth and health (Smail & Lenz, 2024). When a threat (injury, infection, or shift/disturbance in the delicate neural environment) is detected, microglia become activated. During an activated state, microglia change shape and function, with their primary goal being the isolation and clearing of debris. Microglia go to great lengths to eradicate the source of harm, including engulfing and digesting neurons through a process called phagocytosis. While this process can be beneficial, excessive activation can lead to neurodegeneration among other issues.
While most of this chapter has focused on the neurobiology of traumatic stress, a brief discussion of acquired brain injury is merited due to the correlation of head injury among trafficked persons. Traumatic brain injury (TBI) and brain injury by strangulation are two common types of acquired brain injury associated with intimate partner violence and human trafficking. Acquired brain injury can occur due to a bump, blow, or jolt (to the head, neck, or face), penetration of the skull (e.g., stabbing/shooting), forceful or repeated shaking, strangulation, near-drowning, choking, suffocation, etc. (*for a detailed toolbox on brain injury among survivors of IPV see ABI Research Lab, 2025). The severity and symptoms (ABI Toolkit) vary widely and are associated with the brain areas involved, the degree of force/injury, the duration of unconsciousness (if loss of consciousness occurred), and a host of multiecological factors affecting how an individual responds to treatment.
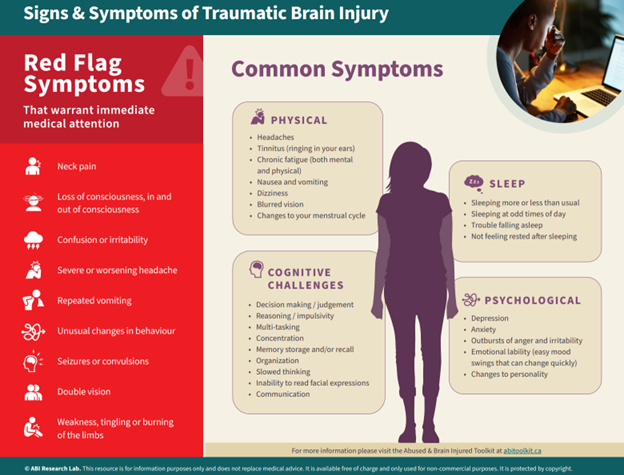
Despite the likelihood of acquiring a brain injury due to IPV and human trafficking, social and structural factors shape professional responses to these types of injuries among trauma survivors. First, symptoms of acquired brain injury can mimic or overlap with symptoms of psychological trauma and mental health symptomology, because, as we have seen in this chapter, the brain can be altered by both physical and psychological threats/injuries. Because of this overlap in symptomology (along with deeply rooted stereotypes), survivors of interpersonal trauma are often dismissed, and their adverse effects are frequently deemed to be “psychological in nature”. Second, the impact of substance use on behavior, mood, and cognition can also distort accurate diagnostics. Imagine how easy it would be to automatically assume a survivor’s depression, anxiety, irritability, difficulty concentrating, or blurred vision was due to their substance use, rather than taking the time to screen for an acquired brain injury. Third, the inherent impact of acquired brain injury can make communicating and recalling symptoms difficult, thus making the history-taking process more challenging. Fourth, disparities in access and utilization of health care can limit a survivor’s opportunities for an accurate diagnosis and treatment. Lastly, systemic biases, lack of training, and lack of awareness related to the co-occurrence of trauma and brain injury continue to result in a highly vulnerable population lacking the appropriate care necessary to prevent further neurological decline.
Neurobiology of Trauma and Social Work Practice – Implications
An awareness of the neurobiology of trauma provides social workers with critical knowledge to support trafficked or formerly trafficked persons in a manner that destigmatizes their experiences and promotes safety, healing, recovery, and resilience. By understanding neuroplasticity and the role various areas of the brain play in traumatic or threatening situations, the social worker is better equipped to appropriately contextualize behavior. Further, a well-informed social worker is positioned to advocate for trafficking survivors who might be misdiagnosed or whose symptoms may be minimized due to their histories. Regarding direct clinical practice, concepts from neuroscience and neuropsychology can support the utilization and implementation of therapeutic modalities that promote homeostasis and the calming of the sympathetic nervous system. Moreover, the biopsychosocial perspective, including a broad understanding of neuroscience, is critical for prevention efforts to combat human trafficking. This perspective provides the social worker with insight into the roots of vulnerability, the neural process at work during a stress response, and the associated traumatic sequelae, as well as a holistic lens through which to provide micro, mezzo, and macro prevention and intervention efforts.
Quiz
Case Study
Alisha
Alisha is a 32-year-old African American survivor of sex trafficking. Her ACE score is 7. During her nine-year trafficking ordeal, Alisha experienced coercive control, strangulation, multiple blows to the head, multiple physical injuries, sexual trauma, and was forced to use drugs. She has been free of her trafficker for eight years and clean for six years. Alisha has engaged in a peer mentoring program and counseling. She has been seeing her primary care doctor for chronic pain. She also complains of having regular headaches, dizziness, and difficulty concentrating, especially when she is tired or when there is a lot of noise or other sensory stimuli. She experiences mood swings and deals with anxiety and depression. Alisha is becoming discouraged because nothing seems to help. Additionally, her primary care doctor brushes off her symptoms, claiming they are psychosomatic (i.e., physical symptoms caused by mental or emotional issues). Despite Alisha being clean, her doctor accuses her of trying to obtain drugs by claiming she is in pain.
Through a biopsychosocial lens, one can appreciate the connections between the body, the mind, and the social environment. Alisha’s nervous system was stressed during childhood (ACE score of 7), altering her neuroinflammatory responses to be more sensitive to threats, which she experienced during her trafficking ordeal. Such sensitivities prime the microglia in an activated state, which increased Alisha’s propensity for neural injury during her trafficking ordeal. Further, her trafficking experiences were prolonged and involved both psychological and physical injuries, leading to structural and functional alterations within her brain. Further, due to prolonged drug use and trauma, Alisha’s brain chemistry has been altered (neurotransmitters). Finally, the instances of strangulation and blows to the head have resulted in an undiagnosed acquired brain injury, causing many of the symptoms Alisha is experiencing. Chronic pain is a common yet overlooked symptom among trauma survivors. It can be attributed to biological and psychological factors (e.g., widespread inflammation, altered areas of the brain responsible for pain perception, neural damage, the body storing traumatic memories, etc.). Because of her history, medical personnel often immediately assume her symptoms are related to psychological trauma or prior substance use. Without an accurate diagnosis and treatment, Alisha will likely experience neurodegeneration and further physical and mental decline as she ages.
Summary of Key Points
- A holistic perspective requires considering biological, psychological, and social factors.
- Basic knowledge of the brain and neural processes enables social workers to better understand and contextualize client behavior, affect, cognition, and health.
Supplemental Learning Materials
American Psychological Association website: https://www.apa.org/
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental
disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787
Kirby, E.D., Glenn, M.J., Sandstrom, N.J., & Williams, C.L. (2024). Introduction to behavioral
neuroscience. OpenStax. https://openstax.org/details/books/introduction-behavioral-neuroscience
Kredlow, M.A., Fenster, R.J., Laurent, E.S., Ressler, K.J., & Phelps, E.A. (2022). Prefrontal
cortex, amygdala, and threat processing: Implications for PTSD. Neuropsychopharmacology, 47, 247-259. https://rdcu.be/eldnc
References
AbuHasan, Q., Reddy, V., & Siddiqui, W. (2023, July 17). Neuroanatomy, Amygdala. In
StatPearls, National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK537102/
American Psychological Association. (2025). Trauma. https://www.apa.org/topics/trauma/
Bremner, J. D. (2006). Traumatic stress: Effects on the brain. Dialogues in Clinical Neuroscience, 8(4), 445–461. https://doi.org/10.31887/DCNS.2006.8.4/jbremner
Cozolino, L. (2024). The neuroscience of psychotherapy. Healing the social brain, fourth edition. Norton Professional Books.
Farmer, R.L. (2009). Neuroscience and social work practice. The missing link. Sage.
Fogwe, L.A., Reddy, V., & Mesfin, F.B. (2023, July 20). Neuroanatomy, Hippocampus.
In StatPearls, National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK482171/
Green D, & McDermott F. (2010). Social work from inside and between complex systems:
Perspectives on person-in-environment for today’s social work. British Journal of Social
Work, 40(8), 2414–2430. https://doi-org.proxy.lib.ohio-state.edu/10.1093/bjsw/bcq056
Hathaway, W.R., & Newton, B.W. (2023, May 29). Neuroanatomy, Prefrontal Cortex. In
StatPearls, National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK499919/
Kirby, E.D., Glenn, M.J., Sandstrom, N.J., & Williams, C.L. (2024). Introduction to behavioral
neuroscience. OpenStax. https://openstax.org/details/books/introduction-behavioral-neuroscience
Leistner, C., & Menke, A. (2020). Hypothalamic-pituitary-adrenal axis and stress. Handbook of
Clinical Neurology, 175, 55–64. https://doi.org/10.1016/B978-0-444-64123-6.00004-7
Levenson, J. (2017). Trauma-informed social work practice. Social Work, 62(2), 105-113.
https://doi.org/10.1093/sw/swx001
Logue, M. W., van Rooij, S. J. H., Dennis, E. L., Davis, S. L., Hayes, J. P., Stevens, J. S., Densmore, M., Haswell, C. C., Ipser, J., Koch, S. B. J., Korgaonkar, M., Lebois, L. A. M., Peverill, M., Baker, J. T., Boedhoe, P. S. W., Frijling, J. L., Gruber, S. A., Harpaz-Rotem, I., Jahanshad, N., Koopowitz, S., … Morey, R. A. (2018). Smaller hippocampal volume in posttraumatic stress disorder: A multisite ENIGMA-PGC study: Subcortical volumetry results from posttraumatic stress disorder consortia. Biological Psychiatry, 83(3), 244–253. https://doi.org/10.1016/j.biopsych.2017.09.006
Matto, H.C., Strolin-Goltzman, J., & Ballan, M.S. (2014). Neuroscience for social work. Current research and practice. Springer Publishing Company.
McEwen, B.S., Gray, J.D., & Nasca, C. (2015). Recognizing resilience: Learning from the effects of stress on the brain. Neurobiology of Stress, 1, 1-11. https://doi.org/10.1016./j.ynstr.2014.09.001
Muroy, S.E., MeeJung K., Jaques, Y., Kaufer, D. (2024). Stress: Neural mechanisms and circuitry of the stress response. In Kirby, E.D., Glenn, M.J., Sandstrom, N., & Williams, C. (Eds.), Introduction to behavioral neuroscience (pp.525-574). OpenStax.
Saraga, M., Fuks, A., & Boudreau, J.D. (2015). George Engel’s epistemology of clinical practice. Perspectives in Biology and Medicine, 57(4), 482-494. https://doi.org/10.1353/pbm.2014.0038
Siegel, D.J. (2012). Pocket guide to interpersonal neurobiology. An integrative handbook of the mind. W.W. Norton & Company.
Siegel, D.J. (2020). The developing mind. How relationships and the brain interact to shape who we are, 3rd ed. Gulford.
Smail, M.A., & Lenz, K.M. (2024). Developmental functions of microglia: Impact of psychosocial and physiological early life stress. Neuropharmacology, 258(1), 110084. https://doi.org/10.1016/j.neuropharm.2024.110084
Wong J.Y.H, Fong, D.Y.T, Lai, V., & Tiwari, A. (2014). Bridging intimate partner violence and the human brain: A literature review. Trauma, Violence, and Abuse, 15(1), 22-33, https://doi.org/10.1177.1524838013496333