Ch. 1: Problems That Commonly Co-occur With Substance Misuse
First, we explore mental/behavioral health challenges that commonly co-occur with substance misuse. The list about which there is available evidence includes:
- mood disorders (e.g., depression, anxiety/panic)
- thought disorders (e.g. schizophrenia and dementia)
- personality disorders
- attention deficit disorder (ADD) with and without hyperactivity (ADHD)
- post-traumatic stress disorder (PTSD)
- risk of suicide
- multiple types of substance use disorder or addictive behaviors (e.g. gambling disorder).
Second, we explore physical health and disability conditions that commonly co-occur with substance misuse, including:
- infectious disease exposure and progression of disease
- non-infectious diseases
- traumatic brain injury
- accidental injury.
As we progress through this module, consider what is meant by co-occurring or concomitant problems. These are issues, concerns, or problems that occur together, are associated with one another, and/or coincide closely in time or over the course of time. When two or more problems coincide like this (they co-occur or are concomitants), several possible models explain the possible relationship between them. Let’s consider examples where Problem A is a form of mental disorder and problem B is an alcohol use disorder.
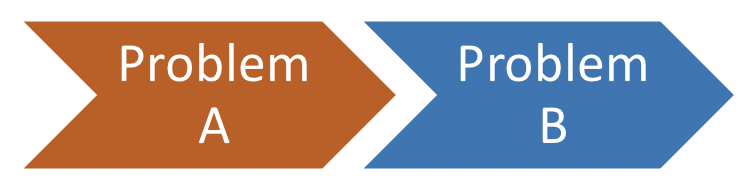 Quite possibly, Problem A causes Problem B, or at least increases the probability that Problem B will arise. For example, mental disorders can contribute to alcohol (or other substance) misuse and use disorder (NIDA, 2018).
Quite possibly, Problem A causes Problem B, or at least increases the probability that Problem B will arise. For example, mental disorders can contribute to alcohol (or other substance) misuse and use disorder (NIDA, 2018).

Or, the opposite may be true: Problem B may cause Problem A. For example, alcohol misuse (or other form of substance misuse) can contribute to the development or expression of mental disorders (NIDA, 2018).
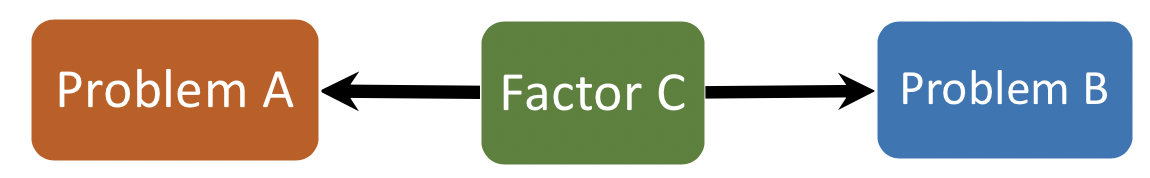 Yet, another possibility is that some third factor influences the emergence of both problems A and B—Problem A does not cause Problem B, nor does Problem B cause Problem A. However, each may be caused or influenced by the same third factor. For example, both alcohol misuse and a mental disorder may be influenced by a common genetic thread or from experiencing violence (e.g. intimate partner violence, sexual assault, child maltreatment, or military combat). Conceptually, this situation exists when both problems (A and B) have shared, common risk or vulnerability factors contributing to their development or expression (NIDA, 2018).
Yet, another possibility is that some third factor influences the emergence of both problems A and B—Problem A does not cause Problem B, nor does Problem B cause Problem A. However, each may be caused or influenced by the same third factor. For example, both alcohol misuse and a mental disorder may be influenced by a common genetic thread or from experiencing violence (e.g. intimate partner violence, sexual assault, child maltreatment, or military combat). Conceptually, this situation exists when both problems (A and B) have shared, common risk or vulnerability factors contributing to their development or expression (NIDA, 2018).
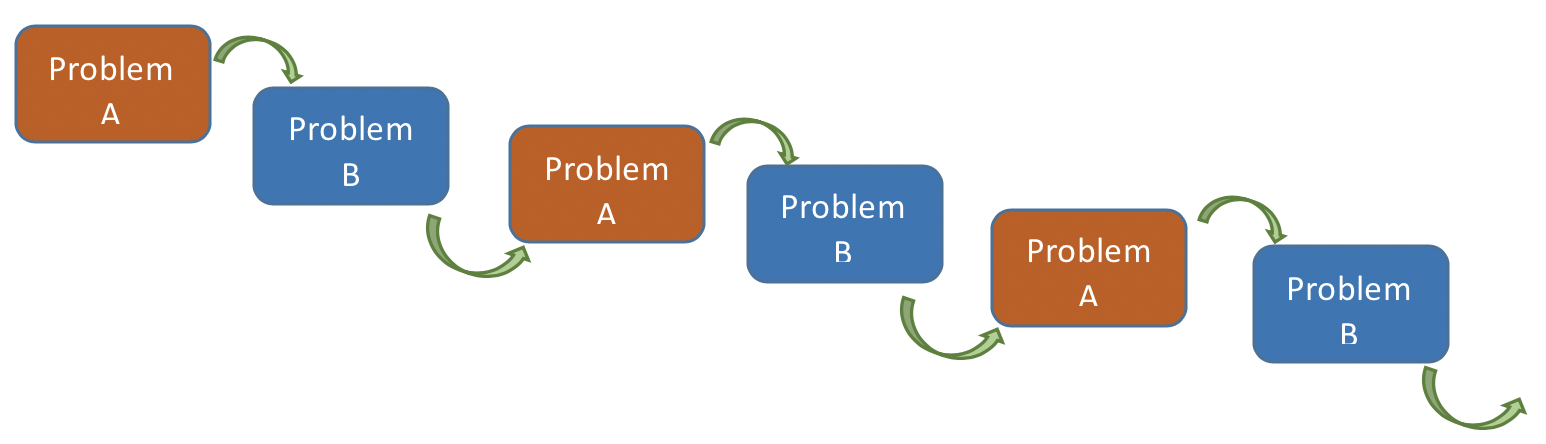
The relationship between problems can be even more complex, including that they are iteratively interacting over time. In other words, Problem A might influence Problem B, which then causes a change (worsening) in Problem A, which then changes Problem B, and so forth over time.
 Why does it matter? Co-occurring disorders and substance misuse/substance use disorders present exceptional life and intervention challenges. “Co-occurring substance use and mental health disorders often present with more severe mental health problems, earlier relapse, greater difficulty maintaining abstinence, more mental health hospitalizations, and greater risk for suicide attempts,” as well as more symptoms of each disorder (Reedy, 2020, p. 529). Having a substance use disorder may mean a person experiences extreme stress and stressor events associated with living “an addicted” life, circumstances that might include homelessness, exposure to violence, and social isolation from friends and family (van Wormer & Davis, 2013, p. 462). The situation is somewhat reminiscent of The Sorcerer’s Apprentice: things were manageable with one or even two brooms but became increasingly challenging as the brooms multiplied.
Why does it matter? Co-occurring disorders and substance misuse/substance use disorders present exceptional life and intervention challenges. “Co-occurring substance use and mental health disorders often present with more severe mental health problems, earlier relapse, greater difficulty maintaining abstinence, more mental health hospitalizations, and greater risk for suicide attempts,” as well as more symptoms of each disorder (Reedy, 2020, p. 529). Having a substance use disorder may mean a person experiences extreme stress and stressor events associated with living “an addicted” life, circumstances that might include homelessness, exposure to violence, and social isolation from friends and family (van Wormer & Davis, 2013, p. 462). The situation is somewhat reminiscent of The Sorcerer’s Apprentice: things were manageable with one or even two brooms but became increasingly challenging as the brooms multiplied.
Unfortunately, individuals with more complex arrays of challenges may be systematically excluded from treatment programs and from research concerning intervention efficacy and effectiveness—these individuals may not meet inclusion criteria by virtue of their exceptional circumstances. Or, one/some of their problems may be masked by the most obvious disorder, rendering appropriate diagnosis and treatment planning difficult. These complexity issues help explain why evidence-based substance-related interventions may fail at higher rates with individuals experiencing co-occurring problems. Let’s look at these commonly co-occurring conditions.
Mental Disorders and Mental Health Challenges
Mental illness is terrifying when it spirals out of control. Repeated alcohol or drug misuse often brings misery, regret, and dire consequences. When the two are combined, the result can be a double whammy of troubles that worsens each condition(van Wormer & Davis, 2013, p. 452).
Based on 2018 National Survey on Drug Use and Health (SAMHSA, 2019a), over 9 million adults aged 18 and older (3.7%) in the U.S. were estimated to have experienced past year co-occurring substance use and mental disorders; for over 3 million (1.3%), their mental disorders were categorized as serious.
The National Co-Morbidity Survey conducted between 2001-2003 involving over 9,000 adults offers some insight into the frequency of co-occurring mental disorders across the U.S., with substance use disorder considered as one form of mental disorder (Kessler et al., 2005). In this report, diagnosable mental conditions were considered co-occurring if they were present during the same 12-month period. Across the sample, 26.2% of participants experienced one or more diagnosable mental disorder. Most often, individuals with a diagnosable mental disorder had only one type (55%), but a considerable number experienced two or more diagnosable mental disorders (45%). The investigators concluded that: “Although mental disorders are widespread, serious cases are concentrated among a relatively small proportion of cases with high comorbidity” (Kessler et al., 2005, p. 617).
| 1 single diagnosis | 2 diagnoses | 3 or more diagnoses |
| 55% | 22% | 23% |
The types of mental disorders that most commonly co-occur with substance misuse and substance use disorder include mood disorders (anxiety, depression, and bipolar disorders), thought disorders (schizophrenia and dementia), personality disorders (including antisocial and borderline personality disorders), impulse control disorders (ADD/ADHD and bipolar disorders), post-traumatic stress disorder (PTSD), and gambling disorder.
Anxiety . Numerous studies have demonstrated that: “Individuals who are more sensitive to symptoms of anxiety may also be more likely to use substances,” particularly alcohol and sedative substances (Reedy, 2020, p. 531). The co-occurrence of anxiety and substance use disorders is “associated with greater symptom severity, higher levels of disability, and poorer course of illness relative to either disorder alone” (McHugh, 2015, p. 99). According to analysis of the National Epidemiologic Survey on Alcohol and Related Conditions III (NESARC) data, alcohol use disorder was modestly associated with panic disorder, phobias, and generalized anxiety disorder, regardless of the level of alcohol use disorder severity (Grant et al., 2015). Concluded from prior NESARC data was that, among individuals experiencing an anxiety disorder, almost 15% experienced a substance use disorder during the past year; additionally, among individuals experiencing a substance use disorder, almost 18% also experienced an anxiety disorder during the past year, and this rose to between 33% to 43% among individuals engaged in treatment (McHugh, 2015).
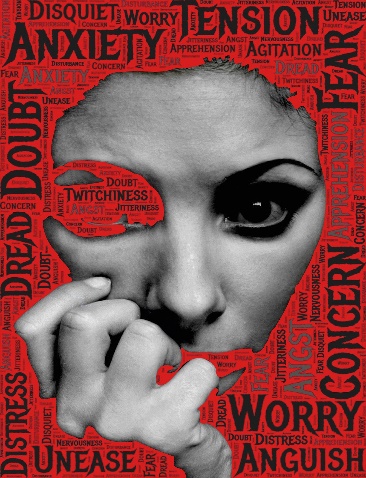 An anxiety or panic disorder differs markedly from the kind of normative anxiety that helps someone function at their peak performance; it is what happens when anxiety becomes intense and unpredictable, is difficult to control, and affects a person’s daily functioning. The experience acute anxiety or panic is both mental and physical, with release of “fight or flight” hormones surging throughout the body, affecting many organ systems. In many instances it is initially difficult to discern between an intense panic attack and a sudden cardiac event (heart attack). The types of anxiety disorder studied in the NESARC-III included panic disorder, generalized anxiety disorder, and phobias (agoraphobia, social, and other specific phobias). It is not surprising that some individuals seek substance-involved solutions to prevent or reduce these intensely disturbing and disruptive anxiety experiences. Recall from prior modules, however, that anxiety also is one possible symptom of some types of substance misuse or withdrawal from some types of substances. For example, anxiety is often experienced during early recovery from alcohol use disorders. It is important through ongoing assessment and diagnosis processes to discern if a person is experiencing anxiety as a primary mental disorder or if what they experience might be substance or withdrawal induced anxiety: “anxiety can be either masked or exacerbated by the effects of substance intoxication, withdrawal, and chronic administration” (McHugh, 2015, p. 3).
An anxiety or panic disorder differs markedly from the kind of normative anxiety that helps someone function at their peak performance; it is what happens when anxiety becomes intense and unpredictable, is difficult to control, and affects a person’s daily functioning. The experience acute anxiety or panic is both mental and physical, with release of “fight or flight” hormones surging throughout the body, affecting many organ systems. In many instances it is initially difficult to discern between an intense panic attack and a sudden cardiac event (heart attack). The types of anxiety disorder studied in the NESARC-III included panic disorder, generalized anxiety disorder, and phobias (agoraphobia, social, and other specific phobias). It is not surprising that some individuals seek substance-involved solutions to prevent or reduce these intensely disturbing and disruptive anxiety experiences. Recall from prior modules, however, that anxiety also is one possible symptom of some types of substance misuse or withdrawal from some types of substances. For example, anxiety is often experienced during early recovery from alcohol use disorders. It is important through ongoing assessment and diagnosis processes to discern if a person is experiencing anxiety as a primary mental disorder or if what they experience might be substance or withdrawal induced anxiety: “anxiety can be either masked or exacerbated by the effects of substance intoxication, withdrawal, and chronic administration” (McHugh, 2015, p. 3).
As far as intervening with individuals who experience co-occurring anxiety and substance use disorders, the literature generally indicates that integrated treatments addressing both anxiety and substance misuse may have superior benefits to separate but concurrent treatment efforts (McHugh, 2015). Pharmacotherapy approaches are available for addressing each disorder but may be less well studied for concurrently addressing both conditions. While exposure therapy for anxiety disorders is somewhat controversial, in situations where an individual also engaged in substance misuse and/or experienced a co-occurring substance use disorder, exposure therapy may not be effective. This conclusion is based primarily on animal studies concerning fear extinction which demonstrated a marked impairment of the fear extinction process following chronic exposure to alcohol, nicotine, morphine (opioid), or cocaine (McHugh, 2015). Mindfulness practices have demonstrated a great deal of promise for supporting management of anxiety disorder symptoms and supporting recovery from substance use disorder, both of which involve mind-physiology aspects (Edguer & Taylor, 2020).
 Depression. Based on a review of literature, investigators concluded that depression may co-occur among as many as 55% to 85% of individuals engaged in treatment for substance use disorders, depending on each study’s methodology and whether the time frame of co-occurrence—at the same time or during the same year (Kingston, Marel, & Mills, 2017). The same literature review concluded that substance use disorder and bipolar disorder co-occurred during the same 12-month period in this population of individuals at about a 10% rate. Authors of the NESARC-III report (Grant et al., 2015) concluded that lifetime alcohol use disorder was significantly associated with persistent depression; among persons with alcohol use disorder, major depressive disorder was the most common of the co-occurring psychiatric disorders (McHugh & Weiss, 2019). Individuals experiencing alcohol use disorder were more than twice as likely to experience past-year major depressive disorder compared to individuals not experiencing alcohol use disorder, and the probability of this co-occurrence increased with alcohol use disorder severity; this association was more prevalent among women than men (McHugh & Weiss, 2019).
Depression. Based on a review of literature, investigators concluded that depression may co-occur among as many as 55% to 85% of individuals engaged in treatment for substance use disorders, depending on each study’s methodology and whether the time frame of co-occurrence—at the same time or during the same year (Kingston, Marel, & Mills, 2017). The same literature review concluded that substance use disorder and bipolar disorder co-occurred during the same 12-month period in this population of individuals at about a 10% rate. Authors of the NESARC-III report (Grant et al., 2015) concluded that lifetime alcohol use disorder was significantly associated with persistent depression; among persons with alcohol use disorder, major depressive disorder was the most common of the co-occurring psychiatric disorders (McHugh & Weiss, 2019). Individuals experiencing alcohol use disorder were more than twice as likely to experience past-year major depressive disorder compared to individuals not experiencing alcohol use disorder, and the probability of this co-occurrence increased with alcohol use disorder severity; this association was more prevalent among women than men (McHugh & Weiss, 2019).
There remains a great deal of confusion in diagnosing alcohol-induced depression versus depression that occurs independently of (but co-occurs with) alcohol use disorder. Intervention strategies under review for concurrently treating co-occurring depression and substance use disorder include pharmacotherapy, combined motivational interviewing and cognitive behavioral therapy, and “transdiagnostic” integrated therapies such as behavioral activation (McHugh & Weiss, 2019). Another reason to explore depression and substance misuse, separate from the comorbidity issue, is that depression is an unfortunately common experience during early recovery from substance misuse/use disorder. “Intoxication and/or withdrawal from certain substances can lead to depressive symptoms…symptoms can last as long as an individual continues to take substances and may or may not improve with abstinence”—lasting up to 6 months of abstinence (CSAT, 2014, p. 7). Depressive symptoms are most likely to occur in relation to chronic use or withdrawal from alcohol, opioids, cocaine and other stimulants, cannabis, or sedative-hypnotic substances (CSAT, 2014).
Depression can interfere with a person’s road to recovery and participation in substance-related intervention efforts. Even if they attend intervention sessions, their depression symptoms may interfere with their ability focus, concentrate, remember, or pay attention during intervention (CSAT, 2014). The Center for Substance Abuse Treatment (CSAT) Treatment Improvement Protocol (TIP) #48 addresses depression during early recovery with the following recommendations:
- screening all substance use treatment participants for depressive symptoms and suicidality;
- being aware of how depressive symptoms appear in persons with substance used disorders and how these might affect treatment participation, process, and outcomes;
- delivering client-centered, integrated treatment for co-occurring depressive symptoms and substance misuse/use disorders;
- delivering evidence-supported interventions (e.g., behavioral, cognitive behavioral, supportive, expressive, 12-step facilitation, and motivational interviewing);
- being aware of how one’s own attitudes toward clients’ depressive symptoms might affect work with these individuals.
“Depression and hopelessness, combined with alcohol and/or drug use, may also increase the potential for violence to self or others. The client may be at higher risk for thinking about, planning, or acting on suicidal thoughts.” (CSAT, 2014, p. 9)
Thought disorder. Both schizophrenia (including schizoaffective and delusional disorders) and dementia are explored under this heading. In these cases, a person experiences episodes during which it is difficult or impossible for them to distinguish between their external and internal worlds—whether the information they are receiving is coming from the outside world or generated in their minds (van Wormer & Davis, 2013).
 Schizophrenia. Early research into the co-occurrence of schizophrenia and substance use disorder estimated that 47% of individuals with schizophrenia also met criteria for a substance use disorder involving alcohol or illicit substances—4.6 times greater than among the general population—and at least 70% of individuals with chronic schizophrenia exhibited nicotine dependence (Winklbaur et al., 2006). The substances most often used by individuals with schizophrenia were alcohol, cannabis, nicotine, and cocaine. Among individuals with schizophrenia, schizoaffective disorder, or bipolar disorder with psychotic features, substance use was significantly more prevalent compared to a comparison group of individuals without severe mental illness (Reedy, 2020).
Schizophrenia. Early research into the co-occurrence of schizophrenia and substance use disorder estimated that 47% of individuals with schizophrenia also met criteria for a substance use disorder involving alcohol or illicit substances—4.6 times greater than among the general population—and at least 70% of individuals with chronic schizophrenia exhibited nicotine dependence (Winklbaur et al., 2006). The substances most often used by individuals with schizophrenia were alcohol, cannabis, nicotine, and cocaine. Among individuals with schizophrenia, schizoaffective disorder, or bipolar disorder with psychotic features, substance use was significantly more prevalent compared to a comparison group of individuals without severe mental illness (Reedy, 2020).
The increased risk of psychosis or psychotic symptoms among some individuals engaging in cannabis misuse was offered as evidence that substance misuse can cause one or more symptoms of mental illness (NIDA, 2010): “in particular, heavy cannabis use may accelerate or exacerbate psychotic symptoms in vulnerable individuals” (Winklbaur et al., 2006, p. 39). There appears to be a genetic basis to this vulnerability (NIDA, 2010). However, the self-medication hypothesis has tended to dominate explanations of high co-occurrence rates: substance misuse may help a person deal with side effects of medications treating schizophrenia symptoms and/or symptoms of the schizophrenia itself (Winklbaur et al., 2006). In addition, the third factor of chronic stress also comes into play: it is a common factor in the severity both of schizophrenia and substance misuse (Winklbaur et al., 2006). And, some reward neural pathways of the brain and neurotransmitters involved in progression to addiction are also involved in schizophrenia symptoms, suggesting that a person with schizophrenia may be more susceptible to have substance use progress to a substance use disorder (Winklbaur et al., 2006).
It can be difficult to tell the difference between behaviors and symptoms caused by substance misuse, withdrawal from substances, and symptoms of a primary thought disorder like schizophrenia. Good assessment, diagnosis, and dynamic evaluation processes are critical to making such a determination and to intervention planning. Complicating treatment for either schizophrenia or substance use disorder is the possibility that either problem will interfere with treatment, leading to significant lapses in treatment and/or increased symptom severity. Additionally, a person with either problem alone or in combination may not engage in adequate self-care—nutrition, hygiene, personal safety and shelter—and may lose/lack social relationships and structures that help keep them functional and able to maintain their health, mental health, and substance recovery. Finally, the misused substance may interact badly or dangerously with medications prescribed for treating schizophrenia. Strong case management practices may be important in supporting individuals who experience co-occurring schizophrenia and substance misuse/substance use disorder.
Dementia. While schizophrenia tends to first appear in younger adults, most forms of dementia tend to first appear during later adulthood. “Dementia refers to a set of symptoms and signs associated with a progressive deterioration of cognitive functions that affects daily activities. Symptoms may include memory loss and difficulties with thinking, problem-solving or language, as well as changes in mood, perception, personality, or behaviour” (Peprah & McCormack, 2019, p. 3). The most common recognized form of dementia is Alzheimer’s disease (Peprah & McCormack, 2019). There exists some evidence to indicate that several types of substance misuse are associated with a higher risk for later development of dementia.
 Prolonged excessive alcohol consumption can lead to permanent changes in brain structures and function, some of which are associated with an alcohol-related form of dementia or diagnosis of Wernicke-Korsakoff syndrome —these may be two distinct syndromes of alcohol-related impairment or they may be variants of the same (Ridley, Draper, & Withall, 2013). Wernicke-Korsakoff syndrome includes some degree of psychosis 80-90% of the time, as well as retrograde amnesia (memory loss), difficulty forming new memories (anterograde amnesia; Martin, Singleton, & Hiller-Sturmhöfel, 2003). The neurological damage and impaired cognition gradually and progressively appear in individuals who have a long history of heavy alcohol misuse. Some behavioral symptoms mimic depression, potentially leading to the erroneous conclusion that an aging person is drinking because of aging-related depression, rather than recognizing that the drinking came first and continued for a long time. If detected early enough, some alcohol-related dementia symptoms can be reversed with proper treatment. A review of literature suggested that alcohol-related dementia may appear at ages younger than many dementia studies include, but across studies the prevalence of alcohol use disorder among individuals with dementia ranges from 9% to 22% and dementia is present in 10% to 24% of individuals with alcohol use disorder (Ridley, Draper, & Withall, 2013).
Prolonged excessive alcohol consumption can lead to permanent changes in brain structures and function, some of which are associated with an alcohol-related form of dementia or diagnosis of Wernicke-Korsakoff syndrome —these may be two distinct syndromes of alcohol-related impairment or they may be variants of the same (Ridley, Draper, & Withall, 2013). Wernicke-Korsakoff syndrome includes some degree of psychosis 80-90% of the time, as well as retrograde amnesia (memory loss), difficulty forming new memories (anterograde amnesia; Martin, Singleton, & Hiller-Sturmhöfel, 2003). The neurological damage and impaired cognition gradually and progressively appear in individuals who have a long history of heavy alcohol misuse. Some behavioral symptoms mimic depression, potentially leading to the erroneous conclusion that an aging person is drinking because of aging-related depression, rather than recognizing that the drinking came first and continued for a long time. If detected early enough, some alcohol-related dementia symptoms can be reversed with proper treatment. A review of literature suggested that alcohol-related dementia may appear at ages younger than many dementia studies include, but across studies the prevalence of alcohol use disorder among individuals with dementia ranges from 9% to 22% and dementia is present in 10% to 24% of individuals with alcohol use disorder (Ridley, Draper, & Withall, 2013).
The evidence surrounding cannabis misuse is less consistent than what we see regarding alcohol misuse. In some studies, long-term heavy cannabis use has been statistically associated with some cognitive deficits involved with dementia later in life—memory, attention, and planful executive functioning tasks have each shown deficits. Shorter term, less frequent cannabis use does not seem to generate the same detrimental effects, and some studies indicated that cannabis use may help slow the progression of some forms of dementia or improve some dementia symptoms—however, the evidence is inconclusive, only suggestive (Peprah & McCormack, 2019).
 Personality disorder. Inflexible, enduring patterns of internal thought processes (cognitions), behavior, affect/emotions, interpersonal relations, or impulse control that lead to significant distress or impairment are encapsulated under the broad category of personality disorder diagnoses (Hassin & Kilcoyne, 2012). Exploring the co-occurrence rates of personality disorders with substance use disorder (and vice versa) is complicated by a bit of pretzel logic since substance misuse is one of the diagnostic criteria for several types of personality disorder.
Personality disorder. Inflexible, enduring patterns of internal thought processes (cognitions), behavior, affect/emotions, interpersonal relations, or impulse control that lead to significant distress or impairment are encapsulated under the broad category of personality disorder diagnoses (Hassin & Kilcoyne, 2012). Exploring the co-occurrence rates of personality disorders with substance use disorder (and vice versa) is complicated by a bit of pretzel logic since substance misuse is one of the diagnostic criteria for several types of personality disorder.
In a review of NESARC data from two periods, antisocial, borderline, and schizotypal personality disorders consistently predicted alcohol, cannabis, and nicotine use disorders; these three personality types also predicted persistence over time (three years) of cannabis misuse, other illicit substance misuse, and prescription drug misuse disorders (Hassin & Kilcoyne, 2012). Additionally, antisocial personality disorder was associated with smoking behavior, not only with nicotine dependence, and obsessive-compulsive personality disorder was associated with drug and nicotine disorders. Of significant concern was the authors’ conclusion that personality disorders predicted poorer course of comorbid substance use (and other mental) disorders. In many instances, a diagnosis of antisocial personality disorder no longer applies after a person is well into recovery—the behaviors and characteristics that warranted the initial antisocial personality disorder diagnosis were part of the survival strategy for maintaining a pattern of substance misuse (van Wormer & Davis, 2013).
Borderline personality disorder is characterized by some of the same traits associated with substance misuse/substance use disorders; similarly, the intoxication or withdrawal phases of substance use are “characterized by features that resemble” borderline personality disorder (Trull et all, 2018, p. 2). The overlaps might include:
- emotion dysregulation, affective instability,
- impulsive acts,
- disturbed interpersonal relationships, interpersonal problems, and
- suicidal/self-harm behaviors (Trull et al., 2018).
Among individuals diagnosed with substance use disorder or receiving treatment for addiction, 22.1% were also diagnosed with borderline personality disorder when multiple studies were considered in combination; about 17% experienced co-occurring alcohol use disorder, and cocaine and opioid dependence occurred at relatively high rates, as well (Trull et al., 2018). The following table is based on data presented in analysis of Revised NESARC data by Trull et al. (2010).
| Personality
Disorder |
% alcohol dependent | % drug
dependent |
% nicotine dependent |
| All types combined | 42% | 19% | 48% |
| schizoid | 38% | 20% | 40% |
| antisocial | 52% | 27% | 59% |
| borderline | 47% | 23% | 54% |
| narcissistic | 39% | 17% | 44% |
| obsessive-compulsive | 32% | 11% | 36% |
Impulse control disorders or ADD/ADHD. Bipolar disorder could have been addressed in the prior section concerning depression and mood disorders, but here it is placed in a category of impulse control disorders. This choice was made because common symptoms of bipolar disorder (mania and impulsivity) also are associated with substance use disorder (Reedy, 2020): “Bipolar disorder has a high co-occurrence with substance abuse disorders” (Post & Kallivas, 2013, p.172). This co-occurrence often appears with more severe bipolar disorder that is more difficult to treat, and there seems to be an iterative sensitization process between them where each episode of either contributes to progression of the other condition (Post & Kalllivas, 2013). Other investigators concluded that alcohol misuse by individuals with bipolar disorder was associated with poorer recovery following their first hospitalization for mania, a greater number of recurrent bipolar episodes and hospitalizations, poorer response to pharmacotherapy, poorer adherence to treatment regimens, and greater progression of an alcohol use disorder (Strakowski et al., 2005). Part of bipolar disorder involves mania, a period during which a person engaged to a great extent in activities which are pleasurable (van Wormer & Davis, 2013)—pleasurable activities which could include substance misuse.
In our prior module concerning CNS stimulants, we introduced the topic of attention deficit disorder with and without hyperactivity—ADD and ADHD. Wilens and Morrison (2011) reviewed the literature concerning the intersection of ADD or ADHD with substance misuse, drawing the following conclusions:
- The rate at which ADHD coincides with substance use disorders is higher than would be expected merely by chance—the rate of ADHD in the general population is about 5-9% but among adults with substance use disorders it is around 25%, and among adolescents with substance use disorders, around 50% have diagnosable ADHD.
- In the group of individuals experiencing substance use disorders, substance misuse generally started earlier among those with ADHD than among those without ADHD. This is relevant because, as you may recall from prior modules, earlier initiation is predictive of more severe problems with substance misuse/use disorder later down the line.
- Since symptoms of ADHD appear much earlier in life than does substance misuse, ADHD appears to influence the emergence of substance use disorder (not the other way around).
- Individuals with ADHD plus conduct disorder and/or bipolar disorder have the greatest probability of developing substance use disorder.
- Early treatment of ADHD with stimulant medication neither increases nor decreases the risk for subsequent substance use disorder; however, it may delay substance use initiation during adolescence.
Again, why does this evidence matter? It should help inform prevention efforts, for one thing. It helps to know where we might want to focus some of our more specific, targeted efforts at prevention, especially our efforts to delay initiation of substance use. It matters because we may need to rethink our substance misuse/use disorder treatment approaches in terms of how well suited they are for a population with ADHD traits. This includes thinking about pharmacotherapy options, particularly medication management (MM) efforts to ensure better compliance with the medication schedule by individuals who have a lifetime of greater difficulty organizing themselves for reliable follow-through.
Trauma. Post-traumatic stress disorder (PTSD) symptoms include difficulties with concentration, attention and focus, along with anxiety and insomnia or sleep disruption. Recalling or psychologically reliving trauma events in dreams and waking memories can be experienced as intensely as the original event—the sympathetic nervous system responds and triggers the “fight or flight” responses of increased heart rate, muscles ready for action, shifting blood sugar levels, heightened blood pressure, and so forth. It takes a while for the parasympathetic system to calm things down again, and a person with PTSD may spend an extreme amount of time in a hyper-vigilant, “ready for action” physiological state. From all that we have learned about the role of neurotransmitters and different regions of the brain regarding substance misuse, we can piece together at least part of the story as to why PTSD and substance misuse might co-occur. The experience of prolonged, chronic stress floods the body and brain with stress hormones and alters brain pathways (e.g. hypothalamus control center and its memory storage areas and the hippocampus and amygdala involved in stress responses). Combined with exposure to various substances, it becomes evident that trauma-related stress can easily lead to substance misuse and substance use disorders.

Early research concerning trauma and PTSD largely stemmed from work with combat veterans. More recently, practitioners and scholars have recognized many of the same trauma-related symptoms (whether or not these meet criteria for a PTSD diagnosis) among numerous other populations, as well: children, adolescents, and adults who have been the target of or witness to family or community violence (e.g., intimate partner violence, sexual assault, child maltreatment); survivors of community-wide natural disasters; and, other survivors of severe and/or life-threatening/life-altering events. The main “take home” lesson from the literature concerning the co-occurrence of trauma/PTSD and substance misuse/substance use disorder is that trauma histories are very common among individuals experiencing substance use disorders.
Combining numerous studies, it appears that alcohol use disorder occurs among 24% to 52% of individuals with PTSD, nicotine dependence among at least 19%, and cannabis use disorder being up to 6 times more common in this population; cocaine use disorder also co-occurred with PTSD at relatively high rates, as did opioid use disorder, particularly among individuals also experiencing chronic pain as a result of trauma (Bailey & Stewart, 2014).
“It is now a well-established fact that there is a surprisingly high degree of overlap between substance misuse and PTSD across diverse community and patient samples. This overlap is of clinical significance because individual with comorbid substance use and PTSD show poorer functioning across various indicators and may alco suffer from worse long-term clinical trajectories” (Read & Oimette, 2014, p. 4).
Just as we learned early in this course about the problem of casually using words like “addiction” and “addicted,” it is equally important to address overly casual use of the term “PTSD” that has crept into our society. Like substance use disorders, PTSD is a very real disorder with debilitating symptoms that also can be effectively treated if properly diagnosed and managed. And, many individuals who experience a traumatic event do not develop symptoms associated with PTSD (Bailey & Stewart, 2014). Trauma related to disaster events and experiences of military veterans are introduced here; intimate partner violence, child maltreatment, and sexual assault are presented in a later section.
 Disaster events. Trauma and PTSD often result from experiencing a disaster event, whether it is a natural disaster (e.g., earthquake, flood, tornado, hurricane, tsunami), health disaster (e.g., epidemic or pandemic), or caused by persons (e.g., terrorist bombing, mass shooting, arson fire). Substance misuse may begin or worsen as a result of disaster exposure. Both immediately and 6 months following the traumatic events that unfolded in New York, Washington DC, and Pennsylvania on 9/11 of 2001, investigators of several different studies identified increased nicotine, alcohol, and cannabis use among residents and first responders/disaster aid workers, with heavy episodic drinking being worse the greater the number of traumatic events and degree of PTSD symptomatology experienced in the aftermath (Bailey & Stewart, 2014). Alcohol misuse increased among first responder firefighters following the Oklahoma City federal building bombing, but primarily those who already experienced an alcohol use disorder; taken together these findings suggest “that increases in substance use may be most strongly related to PTSD status and predisaster substance use” (Bailey & Stewart, 2014, p. 14). Consider also that widespread community disaster events (e.g., Hurricanes Katrina and Rita within one month, or the COVID-19 pandemic) may lead to individuals undergoing unintended, unmanaged (and potentially dangerous) alcohol or other substance withdrawal if the distribution network/supply access is disrupted.
Disaster events. Trauma and PTSD often result from experiencing a disaster event, whether it is a natural disaster (e.g., earthquake, flood, tornado, hurricane, tsunami), health disaster (e.g., epidemic or pandemic), or caused by persons (e.g., terrorist bombing, mass shooting, arson fire). Substance misuse may begin or worsen as a result of disaster exposure. Both immediately and 6 months following the traumatic events that unfolded in New York, Washington DC, and Pennsylvania on 9/11 of 2001, investigators of several different studies identified increased nicotine, alcohol, and cannabis use among residents and first responders/disaster aid workers, with heavy episodic drinking being worse the greater the number of traumatic events and degree of PTSD symptomatology experienced in the aftermath (Bailey & Stewart, 2014). Alcohol misuse increased among first responder firefighters following the Oklahoma City federal building bombing, but primarily those who already experienced an alcohol use disorder; taken together these findings suggest “that increases in substance use may be most strongly related to PTSD status and predisaster substance use” (Bailey & Stewart, 2014, p. 14). Consider also that widespread community disaster events (e.g., Hurricanes Katrina and Rita within one month, or the COVID-19 pandemic) may lead to individuals undergoing unintended, unmanaged (and potentially dangerous) alcohol or other substance withdrawal if the distribution network/supply access is disrupted.
 Military veterans. Practitioners and health care providers are developing an increased awareness and understanding of the stress symptoms exhibited by men and women experiencing exceptional circumstances in military service. Their symptoms may or may not rise to the level of diagnosable post-traumatic stress disorder but may still have profound effects on their lives. In a national survey of U.S. veterans, among those with PTSD (whether combat exposed or not), almost 17% also experienced alcohol use disorder and among veterans with alcohol use disorder, over 20% also experienced PTSD (Norman et al., 2018). Veterans experiencing co-occurring alcohol use disorder and PTSD were more likely than their counterparts with alcohol use disorder alone to have positive screening results for major depression (36.8% versus 2.3%), generalized anxiety disorder (43.5% versus 2.9%), suicidal ideation (39.1% versus 7.0%), or suicide attempt (46.0% versus 4.1%). Their overall quality of life was significantly lower, as well. In other research, cannabis use disorder also was significantly associated with PTSD and depression among veterans receiving services (Reedy, 2020). Estimates of the prevalence for substance use disorder (particularly nicotine, alcohol, and cannabis) among individuals with PTSD exposed to combat ranged between 31% to 76%: combat exposure alone is not the predictive factor, instead it is the experience of PTSD following combat exposure that matters (Bailey & Stewart, 2014). Consider that trauma may be experienced by non-combat members of the military, as well (see sexual assault topic below). Members of the military and military veterans may experience a double threat as far as co-occurring substance misuse and PTSD: not only might they engage in alcohol or other substance misuse as a coping strategy, both internalized and external stigma may impede their willingness/ability to seek behavioral health care (Miller, Pedersen, & Marshall, 2017). Furthermore, they may fear being discharged from their military careers if their difficulties with PTSD and/or substance misuse is discovered.
Military veterans. Practitioners and health care providers are developing an increased awareness and understanding of the stress symptoms exhibited by men and women experiencing exceptional circumstances in military service. Their symptoms may or may not rise to the level of diagnosable post-traumatic stress disorder but may still have profound effects on their lives. In a national survey of U.S. veterans, among those with PTSD (whether combat exposed or not), almost 17% also experienced alcohol use disorder and among veterans with alcohol use disorder, over 20% also experienced PTSD (Norman et al., 2018). Veterans experiencing co-occurring alcohol use disorder and PTSD were more likely than their counterparts with alcohol use disorder alone to have positive screening results for major depression (36.8% versus 2.3%), generalized anxiety disorder (43.5% versus 2.9%), suicidal ideation (39.1% versus 7.0%), or suicide attempt (46.0% versus 4.1%). Their overall quality of life was significantly lower, as well. In other research, cannabis use disorder also was significantly associated with PTSD and depression among veterans receiving services (Reedy, 2020). Estimates of the prevalence for substance use disorder (particularly nicotine, alcohol, and cannabis) among individuals with PTSD exposed to combat ranged between 31% to 76%: combat exposure alone is not the predictive factor, instead it is the experience of PTSD following combat exposure that matters (Bailey & Stewart, 2014). Consider that trauma may be experienced by non-combat members of the military, as well (see sexual assault topic below). Members of the military and military veterans may experience a double threat as far as co-occurring substance misuse and PTSD: not only might they engage in alcohol or other substance misuse as a coping strategy, both internalized and external stigma may impede their willingness/ability to seek behavioral health care (Miller, Pedersen, & Marshall, 2017). Furthermore, they may fear being discharged from their military careers if their difficulties with PTSD and/or substance misuse is discovered.
Gambling disorder. In the DSM-5, gambling disorder is a diagnosable mental disorder with neurobiological similarities to certain substance use disorders (Nower, Mills, & Anthony, 2020). It is defined as “a persistent maladaptive pattern of gambling resulting in clinically significant impairment or distress,” such that an individual exhibits four or more from a set of nine symptoms within a 12-month period, including five that are similar to what is involved in substance use disorder diagnosis (Rash, Weinstock, & Van Patten, 2016, p. 3):
- tolerance—gambling with increasing amounts of money to achieve the desired level of excitement;
- loss of control—unsuccessful attempts to control, limit, or stop gambling;
- withdrawal—restlessness and/or irritability when trying to control gambling;
- negative consequences—risked or lost significant relationships or opportunities because of gambling;
- fixation—preoccupation with gambling-related thoughts (e.g., reliving past gambling experiences, planning future experiences, strategizing ways to fund gambling).
The remaining four are somewhat unique to gambling:
- negative affect—frequently gambles in response to negative affect;
- chasing losses—often follows gambling losses by returning another day in attempt to recoup losses;
- lying—lies about gambling or its consequences;
- bailouts—depends on others for money to alleviate desperate financial situations cause by gambling (p. 4).
 Internet gaming and problematic use of technology has much in common with gambling disorder and internet gaming disorder has been proposed a condition relevant for further study as a diagnosable disorder in the DSM-5; gaming disorder is included in the ICD-11 (Anthony, Mills, & Nower, 2020). As of 2013, the types of gambling in which the largest percent of U.S. adults engaged were (Welte et al., 2015):
Internet gaming and problematic use of technology has much in common with gambling disorder and internet gaming disorder has been proposed a condition relevant for further study as a diagnosable disorder in the DSM-5; gaming disorder is included in the ICD-11 (Anthony, Mills, & Nower, 2020). As of 2013, the types of gambling in which the largest percent of U.S. adults engaged were (Welte et al., 2015):
- lottery (62%)
- office pools/raffles (40.2%)
- casino gambling (26.2%)
- cards, including via internet (19.2%)
- slot machines outside of casino, including via internet (17.4%)
- sports betting, including via internet (16%).
The U.S. prevalence of past year gambling disorder is about 2% and about 3% over the lifetime, however the 6% rate of gambling disorder and 15% for problem gambling is much greater in communities where gambling is integral to economic and social systems (Nower et al., 2020).
The association between gambling disorder and alcohol or other substance use disorder is “well established” (Rash et al., 2016, p. 5): 28% of problem/pathological gamblers experience an alcohol use disorder and 17% experience substance use disorder involving illicit substances. Among individuals seeking treatment for problematic gambling or gambling disorder, over 40% meet criteria for lifetime alcohol use disorder and 21% for substance use disorder involving other substances—including nicotine—and having a lifetime history of substance use disorder is associated with lower rates of achieving gambling abstinence, just as problems with gambling predict poorer substance-related treatment outcomes (Rash et al., 2016). Of interest is the observation that at-risk alcohol use patterns decreased during gambling treatment and incorporating brief alcohol interventions into gambling treatments may further advance these reductions in drinking behavior (Rash et al., 2016). Screening for problematic gambling is recommended for anyone entering treatment for substance use disorder and, vice versa, substance misuse screening is recommended for anyone entering treatment for problematic gambling (Rash et al., 2016). Similarly, ongoing assessment for suicidality is critically important: rates are considerably higher than in the general population—as much as three times more common than in the general population (Nower et al., 2020).
Intervening around co-occurring mental disorders and substance misuse. Both substance misuse and mental disorders can contribute to difficulties in daily living and “generally have a synergistic effect and either can impede treatment of the other,” thus traditional unidimensional sequential or parallel treatment approaches are ill-advised (Reedy, 2020, p. 536). Instead, integrated treatment is recommended for these co-occurring disorders, including when delivered collaboratively by different providers and designed to meet holistic needs over a period of months to years (Reedy, 2020).
Several behavioral therapies judged to have strong evidence supporting their use with co-occurring substance use and mental disorders include (NIDA, 2018):
- cognitive behavioral therapy (CBT)
- dialectical behavioral therapy (DBT)
- assertive community treatment (ACT
- therapeutic communities (TC)
- contingency management (CM).
An evidence-supported model for addressing women’s co-occurring PTSD and substance use disorder was initially presented as Seeking Safety(Najavits, 202).
Pharmacotherapy strategies are also relevant for consideration and may assist in managing one or the other disorder, or perhaps in managing both simultaneously: the example presented by NIDA (2018) is the potential use of bupropion to treat both depression and nicotine dependence. The report also suggests that evidence concerning how these pharmacotherapy agents work singly or in combination for populations experiencing comorbid mental conditions is sorely lacking.
Physical Health
Aside from the risk of accidental overdose, misuse of alcohol, prescription or OTC drugs, and other substances potentially takes a toll on physical health. Substance misuse “contributes to the risk of developing or complicating other illnesses, as well as the substances interacting negatively with medications used to treat medica conditions” and may also impact adherence to medical treatments (Saunders-Adams, Hechmer, Peck, & Murray, 2020, p.438). Integrated health care systems provide behavioral health and substance-related interventions seamlessly within non-stigmatizing settings where a person might be receiving their general, primary health care services (Saunders-Adams et al., 2020). Advocates of integrated care models point to data indicating that substance misuse and substance use disorders are undertreated in the U.S. and globally, with segregation of physical and behavioral health care systems being largely to blame (Saunders-Adams et al., 2020). For example, NSDUH data from 2018 (SAMHSA, 2019a) led to an estimate that over 20 million individuals aged 12 or older (7.4% of population) experienced a past year substance use disorder involving alcohol or illicit use of substances; however, only 3.7 million (1.4% of population) received alcohol or other substance use treatment during that same year. Many more individuals could potentially be identified early in their substance use-use disorder trajectory, supported in recovery, and/or assisted through harm reduction interventions should they enter appropriately prepared integrated healthcare service delivery systems (Saunders-Adams et al., 2020). Physical health concerns that commonly co-occur with different types of substance misuse are worth exploring.
Infectious disease exposure, infection, and disease progression. The significance of “mode of administration” in substance misuse is a theme woven through several modules in this course. The topic is once again relevant because injection administration increases the risk of both exposure to infectious disease and local, injection site infections: viral hepatitis (hepatitis B/HBV, hepatitis C/HCV) and HIV (human immunodeficiency virus), as well as both bacterial and fungal infections (CDC, 2018). Of concern are viruses transmitted through blood or other body fluids present when individuals share drug equipment, including needles (NIDA, 2019). Injection drug use was a contributing factor in their acquiring HIV at a 20% rate among men with the infection (150,000 cases) and 21% among women (50,000), according to 2016 CDC data (NIDA, 2019). Harm reduction practices known as syringe services programs (SSPs) and pharmacies being allowed to sell sterile needles without a prescription are recommended community-based strategies (NIDA, 2019).
 Not only is the concern that someone engaged in injection or non-injection substance misuse might become infected with a disease, but their disease progression and prognosis may be worse, as well. For example, in a study of 1,712 individuals entering care related to HIV infection, “patients with a history of injection drug use were more likely to advance to AIDS or death than non-users”; the researchers detected no statistically significant difference in disease progression between individuals engaged in non-injection drug use and those who did not engage in substance misuse (Qian et al., 2011, p. 14).
Not only is the concern that someone engaged in injection or non-injection substance misuse might become infected with a disease, but their disease progression and prognosis may be worse, as well. For example, in a study of 1,712 individuals entering care related to HIV infection, “patients with a history of injection drug use were more likely to advance to AIDS or death than non-users”; the researchers detected no statistically significant difference in disease progression between individuals engaged in non-injection drug use and those who did not engage in substance misuse (Qian et al., 2011, p. 14).
Furthermore, these infectious diseases can be risk factors in developing other serious health problems or diseases. For example, hepatitis (types B and C) may lead to cirrhosis/loss of liver function and is a significant risk factor in liver cancer (NIDA, 2019); tuberculosis risks include antibiotic resistance, and can affect lungs, brain, kidneys, and spine (https://www.cdc.gov/tb/publications/factsheets/general/tb.htm).Various factors might explain the disease progression phenomenon, but changes in the immune system, as well as a person’s overall health and nutrition status may leave them less able to combat infection or disease. Additionally, substance misuse may worsen the situation: “Drug use can worsen the progression of HIV and its symptoms, especially in the brain. Studies show that drugs can make it easier for HIV to enter the brain and cause greater nerve cell injury and problems” (NIDA, 2019). Individuals engaged in significant levels of substance misuse or experiencing substance use disorder may not receive routine primary health care, testing, and vaccinations that could prevent or minimize the seriousness of infectious diseases; this includes lack of prenatal care among pregnant women.
Individuals engaged in substance misuse, with or without injection use, are also more susceptible to acquiring sexually transmitted infections (STIs) and tuberculosis infection or disease. For example, authors of a literature review concluded that the rate of latent (asymptomatic) tuberculosis among individuals engaged in illicit drug use was 10% to 59% (Deiss, Rodwell, & Garfein, 2009). Also of considerable concern is the increased rate of co-infection between tuberculosis, HIV, and hepatitis (Deiss, 2009). A significant barrier to disease recognition and treatment is the relatively poor access to appropriate primary and specialty care this population experiences (Rodwell, 2009). So too are viruses and other infections sexually transmitted through blood or body fluids, including HIV (NIDA, 2019). Substance use contributes to unsafe sex practices/failure to consistently employ safe sex practices, especially when judgment is impaired, sexual risk is underestimated, or sex is the currency through which the drugs are acquired.
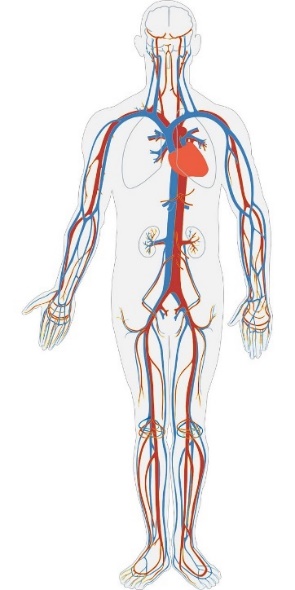 Non-communicable diseases/health complications. As we explored each type of substance, you learned about some of the effects each has on mind, behavior, and health/organ systems. For example, effects on breathing, heart rate/rhythms, blood pressure, immune system, diabetes, stroke risk, fertility/infertility, fetal development, and sleep patterns. Of additional concern is evidence that some types of substance misuse increase the probability of developing cancer.
Non-communicable diseases/health complications. As we explored each type of substance, you learned about some of the effects each has on mind, behavior, and health/organ systems. For example, effects on breathing, heart rate/rhythms, blood pressure, immune system, diabetes, stroke risk, fertility/infertility, fetal development, and sleep patterns. Of additional concern is evidence that some types of substance misuse increase the probability of developing cancer.
- Tobacco products. Among all cancers diagnosed in the U.S., 40% are linked to tobacco use, including cancers of the mouth and throat, esophagus and voice box, lungs, trachea and bronchus, liver, stomach, kidneys/bladder, uterus/cervix, pancreas, colon and rectum, and blood (acute myeloid leukemia) (https://www.cdc.gov/media/releases/2016/p1110-vital-signs-cancer-tobacco.html).
- Alcohol. Alcohol increases the probability of developing cancers of the mouth and throat, esophagus and voice box, liver, colon and rectum, and (for women) breasts, and the risk increases as a function of increased alcohol consumption (https://www.cdc.gov/cancer/alcohol/index.htm). Cancer risk increases even more when alcohol and tobacco are both involved (Saunders-Adams et al., 2020).
- Cannabis. The picture concerning possible cancer risks associated with cannabis/marijuana use is mixed. In a review of literature, authors concluded: “There is currently no consensus on whether marijuana use is associated with cancer risk” (Huang et al., 2015, p. 15). The only consistent evidence they identified suggested that testicular cancer risk increased with frequent marijuana use. Another review drew the same conclusion regarding testicular tumors, and findings for lung cancer were mixed (Ghasemiesfe et al., 2019).
- Sedative-hypnotics. There exists some evidence that regular, prolonged use may contribute to oral, liver, and breast cancer (Fang et al., 2019).
- Opiods. There exists some evidence that regular, prolonged opioid/opiate use may contribute to cancers of the bladder, kidney, oral, esophagus, and larynx/pharynx (Rashidian et al., 2016).
- Anabolic steroids. Steroid misuse typically occurs at high concentrations compared to what is typically prescribed for treating medical conditions; this pattern of misuse is associated with increased risk of developing liver, testicular, prostate, breast, and colon cancers; it is also associated with more aggressive forms of cancer (Tentori & Graziani, 2007).
Not only are these specific substances of concern, so too are possible contaminants and additives that also may be harmful to health—especially drugs that are illicitly manufactured or distributed.
Traumatic brain injury, disability, and other accidental injury. Disability is different from disease in that it concerns long-term mild to severe consequences resulting from injury, disease, genetics, or birth-related circumstances rather than from specific pathogens or disease processes. Substance misuse is an all-too-common cause underlying emergency department visits in the U.S. Estimated based on the Drug Abuse Warning Network (DAWN) 2011 data were 5.1 million drug-related emergency department visits occurred, almost 2.5 million of which were associated with drug misuse or abuse: 51% involved illicit substances, 51% involved nonmedical use of prescription drugs, and over 25% involved drugs combined with alcohol—over 600,000 visits involved drugs combined with alcohol (SAMHSA, 2013). More than 40% of emergency department visits by individuals under the age of 21 involved alcohol (almost 118,000 in this age group involved alcohol alone), particularly among those aged 18-20 years (SAMHSA, 2013).
 “Traumatic brain injury (TBI) and substance abuse (SA) are two of the leading causes of disability” (Sacks et al., 2009, p., 405). Substance misuse is a recognized risk factor for TBI and, vice versa, TBI is a risk factor for substance misuse or substance use disorder; substance misuse also is associated with forms of violence and accidents that result in TBI (Sacks et al, 2009). TBI may result in persistent deficits in executive cognitive functioning, depending on the regions of the brain affected, and this may heighten vulnerability to substance misuse (Bjork & Grant, 2009). Individuals with TBI have demonstrated a propensity to choose immediate small rewards preferentially over delayed larger rewards, and may be impaired in their ability to envision the negative consequences associated with substance misuse, or to recognize their own perception of themselves as having control or self-efficacy over their own behaviors (Bjork & Grant, 2009). These factors not only affect addictive behavior choices, they likely affect recovery and intervention delivery, as well.
“Traumatic brain injury (TBI) and substance abuse (SA) are two of the leading causes of disability” (Sacks et al., 2009, p., 405). Substance misuse is a recognized risk factor for TBI and, vice versa, TBI is a risk factor for substance misuse or substance use disorder; substance misuse also is associated with forms of violence and accidents that result in TBI (Sacks et al, 2009). TBI may result in persistent deficits in executive cognitive functioning, depending on the regions of the brain affected, and this may heighten vulnerability to substance misuse (Bjork & Grant, 2009). Individuals with TBI have demonstrated a propensity to choose immediate small rewards preferentially over delayed larger rewards, and may be impaired in their ability to envision the negative consequences associated with substance misuse, or to recognize their own perception of themselves as having control or self-efficacy over their own behaviors (Bjork & Grant, 2009). These factors not only affect addictive behavior choices, they likely affect recovery and intervention delivery, as well.
Among individuals in treatment for substance use disorders, 38% to 63% also had a traumatic brain injury (Corrigan et al., 2005). Screening for both TBI and substance misuse is relevant because each complicates the course of treatment for the other (Sacks et al., 2009). It is important to recognize that TBI may not occur all at once, in one severe event, but may result from an accumulation of less severe events; mild TBI represents up to 90% of all TBIs, and more than 60% of individuals experiencing repetitive mild TBI do not seek medical care (Haycraft & Glover, 2018). For example, in a study of 845 individuals entering treatment for alcohol or other substance use services, 54% had positive screening results for a prior TBI (Sacks et al, 2009). Only 24% of participants reported not having received any blows to the head while over 50% reported having received more than two blows to the head and more than 25% reported more than four; sports-related injuries were the most common source (18%), with assault (14.5%), motor vehicle accidents (13%), falls during drug/alcohol blackout (9%), and other falls (12%) also commonly represented. The authors recommend multifaceted (integrated) treatment addressing substance misuse as well as cognitive remediation and addressing emotional and behavioral aspects associated with TBI. They go on to say that individuals with cognitive deficits associated with TBI may be unable to effectively engage in traditionally delivered substance-related treatment programs and relying on narrowly focused approaches result in treatment failure and relapse:
“For these individuals, strategies to facilitate compensation for these cognitive deficits need to be incorporated as core components of their [substance abuse] treatment (e.g., allowing for more repetition of information, prompting individuals to write things down to aid in memory for information, use of memory books, extended treatment duration)” (Sacks et al., 2019, p. 413).
Driving under the influence (DUI). Depending on the state or local jurisdiction, the offense of impaired, drugged, or drunk driving may be called:
- driving under the influence (DUI),
- driving while intoxicated (DWI),
- driving while impaired (DWI),
- operating (a vehicle) under the influence (OUI), or
- operating (a vehicle) while intoxicated (OWI).
As noted in our module focused on alcohol, even if a person’s blood alcohol level (BAL)/blood alcohol concentration (BAC) does not measure at the legal limit (0.08%), performing the complex array of tasks involved in driving still may be impaired. Impairment may also occur with other legal prescription and OTC substances, as well as an array of illicit substances. The odds of driving accidents increase sharply with increasing BAC levels, according to calculations presented by the World Health Organization (WHO, 2009)—any fraction over the value of 1.0 is an increased risk (“buzzed driving is drunk driving”):
| BAC range | Odds Ratio |
| 0.01% – 0.04% | 1.17 |
| 0.05% – 0.07% | 1.71 |
| 0.08%* -0.10% | 3.93 |
| 0.11% or greater | 10.68 |
| *legal limit in U.S. |
The 2018 NSDUH data (SAMHSA, 2019a) led to estimates that over 20 million individuals aged 16 and older (8%) drove under the influence of alcohol during the past year, and 12 million (4.9%) under the influence of illicit substances—most often, marijuana (11.8 million, 4%).
News reports in recent years have identified car crashes where legal non-benzodiazepine sleep medications (e.g. Ambien®) were reportedly involved. While it is clear to most of us that driving under the influence of alcohol, marijuana, or (other) illicit substances is a bad idea (and illegal), it is dangerous to overlook the potential dangers associated with driving under the influence of (other) legal OTC and prescription substances. The Automobile Association of America (AAA, 2014) reported that, while 66% of people consider driving under the influence of alcohol to be a very serious threat and 56% considered driving under the influence of illegal drugs to be so, only 28% consider driving under the influence of prescription drugs a very serious threat. They reported that the crash risk increased by up to 41% when driving under the influence of certain antidepressants and that even over-the-counter cold and allergy medications can impair driving. The AAA Foundation for Road Safety hosts an interactive informational site where specific prescription and OTC medications can be searched for potential drug interactions, food interactions, driver warnings, and general medication information: http://www.roadwiserx.com/. Dangers also apply to operating any dangerous equipment, not only motor vehicles (e.g. boats, snow mobiles, riding mowers, planes, and industrial/construction machinery).

STOP & THINK
