Ch. 1: What Are Stimulant Substances and Their Effects?
In a previous module we examined central nervous system (CNS) depressants; this time we are looking at their opposite, the CNS stimulants. There exist many forms of stimulant substances, some of which are legal and unregulated in the United States (like coffee and tea), semi-regulated (like age restrictions on tobacco and vaping/e-cigarette products and stimulant medications requiring health provider prescriptions), or highly regulated (like methamphetamine which is illegal to manufacture, distribute, or possess). Many stimulant substances are synthetically produced; many others occur in nature and may have been used by humans from different cultures for hundreds or even thousands of years for their ability to increase alertness, attention, and energy. For example, local practices of chewing betel nuts (practiced in some Asian/Pacific areas) or coca leaves (practiced in parts of South America) are not usually included in reports of psychoactive substance use/misuse, despite these practices having potentially significant public health consequences, such as oral cancers (Begun, 2020). In this chapter we explore the most commonly used and misused of the stimulant substances, keeping in mind that worldwide there are many, many more (e.g., khat and bath salts) that we will not explore. Before we examine specific types of stimulant substances, let’s look at the common effects these substances generally produce, then we can look more specifically at their differences.

Effects of Stimulant Substances
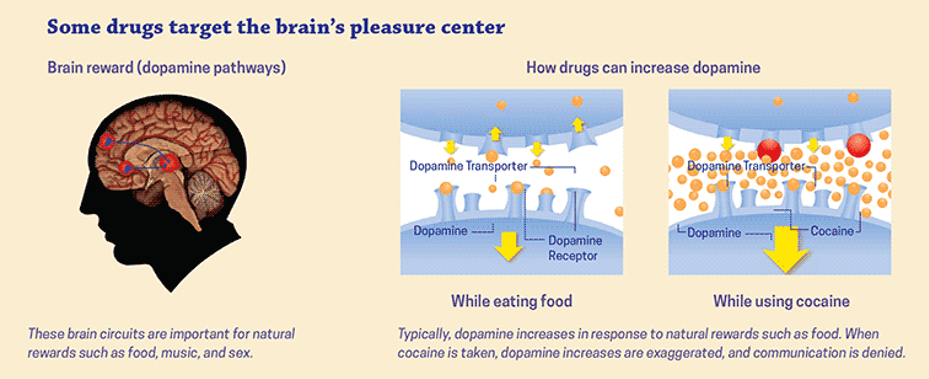
Despite their many differences, stimulant substances share some common effects. Furthermore, when combined, their effects may be amplified—including their side effects (Begun, 2020). Stimulants produce their psychoactive effects through some or all of four major neurotransmitters: serotonin, dopamine, epinephrine, and norepinephrine. Serotonin and dopamine have appeared in several of our previous modules concerning psychoactive substances, so that should be no surprise. We have not previously much encountered epinephrine and norepinephrine in conjunction with other substances. These two substances have a great deal to do with the process we previously studied where the brain (and other organ systems in the body) attempts to maintain a state of homeostasis. The system responsible for controlling many physiological functions throughout the body, ones we do not have to think about, is called the autonomic nervous system (ANS). This includes maintaining proper breathing, heartrate, blood pressure, body temperature, sweating, digestion, and kidney/urinary functions. The autonomic nervous system regulates these functions under dynamic, changing internal and external circumstances through two complementary divisions: the sympathetic and parasympathetic nervous systems.
The sympathetic nervous system usually runs things at a relatively even baseline level while the person is functioning within a normal operational state. The sympathetic nervous system, however, is prepared to gear up, creating a rapid “fight or flight” stress response to perceived threats, events, or stimuli. Once the system is all revved up and the threat has passed, the system needs to calm back down again. That is where the parasympathetic nervous system engages and helps bring the body back to its homeostatic resting baseline state again.

How do stimulant substances play a role in all of this arousal and becalming balance dance? Most stimulant substances trigger the sympathetic nervous system to a state of arousal, as if an event warranting a “fight or flight” stress response truly exists. They do this through their influence on two neurotransmitters, epinephrine and norepinephrine. Together these two neurotransmitters play a role in the body’s stress response; epinephrine is also known as adrenaline and norepinephrine as noradrenaline. Just as we have previously discussed in comparing endogenous (naturally occurring internal sources) and exogenous (introduced from the outside) substances, use of stimulants can cause release of these neurotransmitters in much greater quantity; additionally, some impede neurotransmitter reabsorption so they hang around in the “active” synaptic gap/cleft for an extended duration. This, in turn, keeps the person in a higher state of arousal far longer than nature might have intended as a helpful “fight or flight” response.
The major psychoactive effects across the class of stimulant substances include possible:
- heightened state of alertness, attention, and focus
- wakefulness
- feelings of pleasure, euphoria, enhanced mood (dopamine reward system activity)
- restlessness, nervousness, anxiety, agitation, and jittery feelings
- increased sexual libido
- irritability, aggressiveness, and paranoia
- hallucinations.
Because of their psychoactive effects, stimulant substances are sometimes used in combination with some of the other substances studied in our course. For example, individuals may engage in polydrug use involving stimulants to counter undesirable effects of other substances, such as combining cocaine or methamphetamine with heroin. A potentially problematic trend that has even proven fatal involves combining stimulants (e.g., caffeinated/stimulant beverages) with alcohol in an attempt to delay onset of warning signs from drinking too much too fast—this, in turn, contributes to alcohol poisoning.
In addition to their psychoactive effects, stimulant substances affect multiple organ systems, thus they can have multiple side effects. In addition to mood swings, irritability, and paranoia, side effects of stimulant use might include:
- accelerated heart rate, blood pressure, and body temperature (especially with physical activity), as well as increased blood sugar
- reduced blood flow to many organs
- appetite suppression
- disrupted sleep patterns
- growth retardation/slowed physical development in fetuses, children, and adolescents
- tremors
- seizures
- amphetamine-induced psychosis.
 Stimulant misuse can be risky because of the cardiac (irregular and accelerated heart rate), elevated blood pressure, and elevated body temperature effects. Many stimulant substances are potentially addictive, some with greater addictive potential than others. Individuals do develop tolerance to many forms of stimulant substances and may experience withdrawal symptoms with discontinued use following a period of regular use. Consider how you or others you know describe feeling when they miss their routine coffee or it has been a lengthy period of time since their last cigarette. Withdrawal from any stimulant substance might include fatigue, headaches, depression, and disrupted sleep patterns. The effects may be more intense in withdrawal from some substances compared to others; however, stimulant withdrawal lacks the medical risks associated with alcohol and CNS depressant withdrawal.
Stimulant misuse can be risky because of the cardiac (irregular and accelerated heart rate), elevated blood pressure, and elevated body temperature effects. Many stimulant substances are potentially addictive, some with greater addictive potential than others. Individuals do develop tolerance to many forms of stimulant substances and may experience withdrawal symptoms with discontinued use following a period of regular use. Consider how you or others you know describe feeling when they miss their routine coffee or it has been a lengthy period of time since their last cigarette. Withdrawal from any stimulant substance might include fatigue, headaches, depression, and disrupted sleep patterns. The effects may be more intense in withdrawal from some substances compared to others; however, stimulant withdrawal lacks the medical risks associated with alcohol and CNS depressant withdrawal.
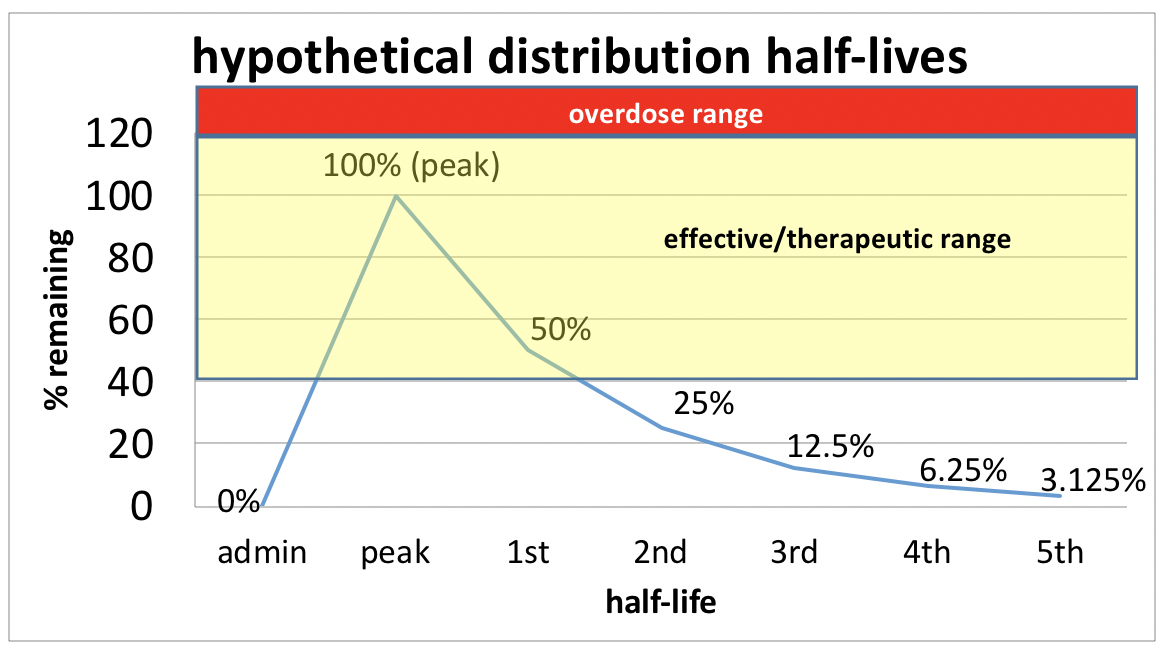
Another problem with many stimulant substances is the mood swing (emotional “crash”) that can occur as a dose wears off, before the next dose is scheduled—a rebound effect. Recalling what you learned about the pharmacokinetics of different medications (Module 3), there exists a zone around which the circulating drug dose achieves therapeutic effects; too high and the risk of overdose or negative side effects rises, too low and the amount circulating in the body cannot have the desired effect—it is below the therapeutic threshold. As stimulant substances are metabolized and the circulating dose drops, individuals may experience a precipitous emotional mood swing where negative emotions (irritability and depressed mood) become overwhelming and difficult to control as the drug “washes out” of their system. While this could be relieved by taking the next dose of medication or using more of the stimulant substance, combined with what remains in the body could exceed the safety zone (risking overdose). In addition, managing stimulant medication schedules is complicated by timing issues: for example, appetite suppression effects mean the person should not take/use it prior to mealtime and the alert/wakefulness effects mean the person should not take use it too late or before bed. Many stimulant substances have relatively short half-lives, so they quickly “wash out” of the system. Some medications (e.g., Ritalin®) come in slow, extended, or time release versions which may “soften the crash” experience.
Different Types of Stimulant Substances
At this point, let’s look at specific characteristics and uses/misuses associated with different types of stimulant substances. Here we consider amphetamines (including methamphetamine), cocaine, caffeine, and nicotine (including tobacco and vaping/e-cigarette products). In each case, the previously discussed effects remain relevant. Additionally, in each case, the mode of administration matters, too: injection reaches the brain more quickly than ingestion (swallowing), and along with “snorting” and inhaling may have a stronger influence on addictive potential. Furthermore, injection use has associated infectious disease and infection harm risks.
Amphetamines.
Amphetamines are synthetically produced drugs that are a subject of concern related to prescription abuse (along with opioids). Common prescription drugs of this type include dextroamphateamine (Dexedrine® and Adderall®) and methlphenidate (Ritalin® and Concerta®). Some of the common “street” names include bennies (referring to benzadrine), black beauties, study drugs, speed, uppers, and vitamin R (a reference to Ritalin®). These types of drugs are typically prescribed in managing attention deficit disorder (ADD) and attention deficit hyperactivity disorder (ADHD), and less often for narcolepsy, some forms of depression, and some respiratory problems (including asthma). At times, certain amphetamines have also been prescribed for weight management or weight loss purposes, and the military historically distributed amphetamines to troops to help them stay alert and awake for long hours (Rasmussen, 2008). Typically, these drugs are swallowed, but can be crushed and “snorted,” smoked, or injected.
The tendency to develop tolerance and significant side effects associated with the prolonged use of amphetamines, including their considerable addictive potential, has contributed to reconsideration of their recommended medical uses. Amphetamine misuse is one significant aspect of prescription abuse concerns. First, a person misusing these drugs may not gain the same benefits as someone for whom they are prescribed and risks their negative effects. Second, the person for whom they were prescribed is not taking them, therefore is not gaining the anticipated therapeutic benefits.
According to the UNODC report in 2010, clandestine laboratories producing amphetamines were detected in 32 countries. The greatest number were located in the U.S., Canada, Mexico, China, Australia/New Zealand, and several additional European countries.
 The stimulant paradox with ADD/ADHD. Why would stimulant medication be prescribed to manage ADD or ADHD? On the surface, it seems rather paradoxical or counter-intuitive to provide stimulants to someone who already naturally exhibits high levels of energy and activity—a bit like adding fuel to an already burning fire. Use of medications like Ritalin®, Concerta®, Adderall®, and Dexedrine® increases dopamine levels in the brain, a neurotransmitter responsible for cognitive alertness (among other things). This dopamine release improves attention, motivation, and ability to focus. In turn, this directly helps the person with ADD/ADHD improve in a whole lot of performance areas, but it also helps through a more indirect route, as well. For example, it can improve a their ability to respond appropriately to social cues, stay on task in school or work activities, and control their impulsiveness, all of which can positively influence social relationships, self-esteem, self-confidence, and self-image. In some instances, stimulant medication may also increase activity in areas of the brain that help a person inhibit their actions (behavioral control centers). However, medication alone is not sufficient to successfully manage ADD or ADHD: a great deal of hard work is also involved in learning appropriate coping and self-management skills (behavioral coping). Stimulant medication may provide someone with a better chance for behavioral interventions to be more effective. Without medication, it is more difficult (but not impossible) for a person with ADD or ADHD to generate the focused attention needed to learn these new intentional behaviors and skills.
The stimulant paradox with ADD/ADHD. Why would stimulant medication be prescribed to manage ADD or ADHD? On the surface, it seems rather paradoxical or counter-intuitive to provide stimulants to someone who already naturally exhibits high levels of energy and activity—a bit like adding fuel to an already burning fire. Use of medications like Ritalin®, Concerta®, Adderall®, and Dexedrine® increases dopamine levels in the brain, a neurotransmitter responsible for cognitive alertness (among other things). This dopamine release improves attention, motivation, and ability to focus. In turn, this directly helps the person with ADD/ADHD improve in a whole lot of performance areas, but it also helps through a more indirect route, as well. For example, it can improve a their ability to respond appropriately to social cues, stay on task in school or work activities, and control their impulsiveness, all of which can positively influence social relationships, self-esteem, self-confidence, and self-image. In some instances, stimulant medication may also increase activity in areas of the brain that help a person inhibit their actions (behavioral control centers). However, medication alone is not sufficient to successfully manage ADD or ADHD: a great deal of hard work is also involved in learning appropriate coping and self-management skills (behavioral coping). Stimulant medication may provide someone with a better chance for behavioral interventions to be more effective. Without medication, it is more difficult (but not impossible) for a person with ADD or ADHD to generate the focused attention needed to learn these new intentional behaviors and skills.
Individuals with ADD or ADHD vary widely in their level of response and improvement (cognitive and behavioral) with stimulant medication—some improve dramatically, others only slightly, and some not at all. Some experience better outcomes with one type of stimulant medication than with another, while other individuals do better with different medications. In addition, medications may need to be switched if a person develops tolerance to one that previously provided good outcomes. Systematically tested evidence indicates that cognitive performance is not enhanced in individuals who do not have ADD or ADHD—despite widespread popular beliefs (NIDA, 2018). However, a person may have greater wakefulness which may allow a chance to study longer, which contributes to an elevate rate of prescription amphetamine misuse by high school and college students—it does not make them “smarter.” Use of these stimulant drugs by individuals without primary ADD or ADHD can stimulate hyperactivity while the drug is in their system. And, of great concern with this form of amphetamine prescription misuse: substances with the effect of increasing dopamine also have an increased probability of addiction because of the drug’s effects on the pleasure centers of the brain.
The National Institute on Drug Abuse (NIDA, 2018, however, summarizes data concerning individuals who do have ADD or ADHD and use stimulant medication as prescribed:
Some people may be concerned about later substance misuse in children and teens who’ve been prescribed stimulant drugs to treat ADHD. Studies so far have not shown a difference in later substance use in young people with ADHD treated with prescription stimulants compared with those who didn’t receive such treatment. This suggests that treatment with ADHD medication does not positively or negatively affect a person’s risk of developing problem use.
Methamphetamine.
 Methamphetamine is a specific form of synthetically manufactured amphetamine. Vast amounts of methamphetamine are produced in illegal, foreign, or clandestine labs (Begun, 2020). Not only is methamphetamine a controlled substance (Schedule II in the U.S. DEA system), many of the ingredients used in its manufacture are also controlled substances making it illegal to distribute or possess in excessive amounts. This is why U.S. pharmacies record and limit the amount of pseudoephedrine over-the-counter product a person attempts to purchase (e.g., Sudafed® and Contac®). Methamphetamine “street” names include meth, ice, crystal, crystal meth, and glass (Stoneberg, Shukla, & Magness, 2018; https://www.justice.gov/archive/ndic/pubs5/5049/5049p.pdf).
Methamphetamine is a specific form of synthetically manufactured amphetamine. Vast amounts of methamphetamine are produced in illegal, foreign, or clandestine labs (Begun, 2020). Not only is methamphetamine a controlled substance (Schedule II in the U.S. DEA system), many of the ingredients used in its manufacture are also controlled substances making it illegal to distribute or possess in excessive amounts. This is why U.S. pharmacies record and limit the amount of pseudoephedrine over-the-counter product a person attempts to purchase (e.g., Sudafed® and Contac®). Methamphetamine “street” names include meth, ice, crystal, crystal meth, and glass (Stoneberg, Shukla, & Magness, 2018; https://www.justice.gov/archive/ndic/pubs5/5049/5049p.pdf).
Because of its rapid effect on dopamine release in the brain’s reward system (it is a smoked substance), methamphetamine has high addictive potential (NIDA, 2019a). It also has a relatively long half-life period, meaning that the “high” associated with its use may last 12 or more hours (https://www.justice.gov/archive/ndic/pubs5/5049/5049p.pdf). Individuals sometimes engage in binge use (sometimes called “tweaking” or “a run”) which involves repeated dosing over a period of days in an attempt to maintain the “high” from its use. “Because the pleasurable effects of methamphetamine disappear even before the drug concentration in the blood falls significantly, users try to maintain the high by taking more of the drug,” sometimes foregoing food and sleep for several days while continuing to take the drug (NIDA, 2019b).
Tolerance may develop in both the relatively short term and long term with repetitive methamphetamine use (https://www.ncbi.nlm.nih.gov/books/NBK64328/). Repeated use also may produce drug sensitization—a term to describe a sort of reverse tolerance phenomenon. Sensitization involves the development of hypersensitivity to the effects of a drug like methamphetamine (Ujike & Sato, 2004). This process may be related to the neurotoxic effects of methamphetamine whereby neuronal dopamine storage vesicles rupture and dopamine leaks into synapses and inside the neurons themselves (https://www.ncbi.nlm.nih.gov/books/NBK64328/). In other words, it takes less of the drug to cause some of the psychoactive effects previously experienced at higher doses. And, just as cross-tolerance can develop, so too can cross-sensitization: it may be that a person will develop the same sensitization response to other substances in the same class/type as the one to which sensitization initially developed, although cross-sensitization may also affect drugs in a different class (Stewart & Badiani, 1993). It is exceedingly difficult to anticipate whether an individual person using a specific substance will develop tolerance or sensitization as a result of “chronic” use (Stewart & Badiani, 1993).
In addition to the risks associated with any stimulant misuse, methamphetamine use is associated with an increased risk of stroke. Magnetic resonance imaging (MRI) studies indicate that regular methamphetamine use is associated with a reduction in the density of grey matter in areas of the brain responsible for certain mental functions, and a significant amount of gray matter recovery is observed in individuals who remain abstinent for at least 6 months (Fowler, Volkow, Kassed, & Chang, 2007). After at least 9 months of methamphetamine abstinence, the number of dopamine transporters available in the brain may have increased again, more closely resembling the number in persons who did not use this drug, but poor memory and slowed motor deficits are not repaired (Fowler et al., 2007). According to the American Dental Association, methamphetamine use can have devastating effects on a person’s dental health, resulting in severe tooth decay and gum disease, broken teeth, and tooth loss, sometimes called “meth mouth” (https://www.mouthhealthy.org/en/az-topics/m/meth-mouth). Additionally, methamphetamine may induce changes in the immune system which can worsen the consequences/severity of infectious diseases (e.g., HIV) if they are contracted (NIDA, 2019a).
Methamphetamine production introduces safety concerns over and above those related to all illicit drug distribution (“dealing”) activities. Numerous serious and explosive fires are attributed to “meth lab” errors which not only affect those involved in the illicit production of methamphetamine, but also neighbors, first responders, and whole communities.
The chemicals used to produce methamphetamine are extremely hazardous. Some are highly volatile and may ignite or explode if mixed or stored improperly. Fire and explosion pose risk not only to the individuals producing the drug but also to anyone in the surrounding area, including children, neighbors, and passersby. https://www.justice.gov/archive/ndic/pubs7/7341/7341p.pdf)
In addition, exposure to the toxic chemicals involved in production of methamphetamine poses significant health risks to the individuals involved in production, as well as to others unknowingly exposed—again, including neighbors, first responders, and whole communities. Trash resulting from production efforts often is heavily contaminated with toxins and polluted waste contaminates the production site. Entire buildings/houses may become contaminated with particulate contaminants spread through ventilation systems, making the site dangerous to unsuspecting occupants. Cleanup of a “meth lab” site often requires expensive and extensive hazardous material procedures. Recent statistics suggest that methamphetamine manufacture across the U.S. has declined as more of the drug is smuggled into the country, most from Mexico (Vestal, 2017). Historical data once suggested that methamphetamine use was more problematic in rural communities; current data indicate that this is no longer the case— methamphetamine use has moved into other, more urban communities, as well (Vestal, 2017).
Cocaine.
Cocaine is a stimulant substance that also has anesthetic properties and a long history of use (and misuse) in the United States. It is derived from a naturally occurring source: plants in the erythroxylum group that include coca, laetervirens, and novogranatense varients. (Note that coca and cacao plants are different, see caffeine section below.) Cocaine has various “street names,” some of which relate to different forms (powder or crystal): for example, coke, crack, blow, and snow. “Freebasing” refers to heating and smoking a processed crystal form of cocaine (crack). “Speedballing” refers to the practice of combining cocaine with heroin which increases the risk of heroin overdose because the initial effects of the cocaine (a stimulant) offset the sedating effects of the heroin, encouraging higher doses of heroin to be used; as the cocaine wears off quickly, the respiratory effects of the heroin predominate, leading to an overdose outcome (NIDA, 2016).
Common methods of cocaine administration lead to quick and intense psychoactive effects; it is usually “snorted,” smoked, or injected, but may be rubbed on gums to be absorbed. As with many other potentially addictive substances we have studied in this course, the intensity of the dopamine (brain reward) response to cocaine is far greater than is elicited endogenously from engaging in natural pleasure behaviors (https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drugs-brain). The historical advertisement here refers to cocaine dissolved in solution intended to be applied (and absorbed) on the gums of a person experiencing dental pain or the gums of babies and young children experiencing pain associated with teething.
Cocaine is a quickly metabolized substance (short half-life), so its psychoactive effects tend to be short-lived (https://www.ncbi.nlm.nih.gov/books/NBK64328/). While the “high” cocaine use produces occurs quickly, the effect also fades quickly, within minutes to an hour (NIDA, 2016). The duration of effect is somewhat dependent on route of administration: “The faster the drug is absorbed, the more intense the resulting high, but also the shorter its duration” (NIDA, 2016). In addition, like many stimulant substances, cocaine tolerance develops readily and individuals experience rebound effects after repetitive use—“the crash” after the high.
Bleeding within the brain and stroke have been associated with cocaine use, and long-term cocaine use is associated with a wide range of cognitive deficits in attention, memory, impulse control, and motor actions (NIDA, 2016). Gray matter density loss in the frontal cortex of the brain (responsible for logical thinking, goal setting, planning, and self-control, among other functions) is observed on MRI scans of individuals who have engaged in chronic cocaine misuse ((Fowler et al., 2007)). The physiological effects of cocaine use on other organ systems include cardiac arrest or seizures, the two most common causes of cocaine-related death (NIDA, 2016). The avenue of use may also increase risks of other health complications, such as infectious disease exposure and infections associated with injection use, or nasal passage deformations from “snorting” cocaine. Tolerance and withdrawal may develop with regular cocaine use, contributing to continued use in order to avoid or relieve withdrawal symptoms and requiring increasingly greater doses to do so.
Caffeine.
Caffeine is included in this chapter because it is believed to be the stimulant (possibly the “drug”) most widely used globally (NIDA, 2014). “According to the Dietary Guidelines for Americans 2015-2020, more than 95 percent of adults in the United States consume foods and drinks containing caffeine. On average, U.S. adults consume between 110 and 260 milligrams (mg) of caffeine per day” (https://www.medicalnewstoday.com/articles/324986).
Caffeine is present in many forms of tea, coffee, chocolate, and “energy” products. Decaffeinated coffee, despite what the name suggests, retains some caffeine content although at low amounts; the word is not to be confused with caffeine-free (no caffeine). One problem with comparison of caffeine content across types and brands of caffeinated producs is that serving sizes are often not comparable. For example, a “cup” of coffee might be 6 or 8 ounces, and in terms of specialty coffees like those produced by Starbucks®, serving sizes (8, 10, 12, 16, 20, 24 and 31 ounce containers) are confounded by what else is added (milk, sugars/syrups, and other flavor vehicles). Comparing soft drinks is equally confounded by serving size. For example, in the U.S., small, medium, and large beverages served at McDonald’s are 16, 21, and 32 ounces respectively; small, medium, large, and extra-large beverages served at Burger King are 16, 20, 29, and 38 ounces respectively. (There are significant sizing differences in other countries.)
While caffeine content may be presented per 8 ounces, most containers are consumed as a single serving despite the labeling reference to 2 or more servings per container. This harkens back to the “standard drink equivalent” problem we saw in our focus on alcohol module. (A table is presented below comparing caffeine content from various different sources with corresponding serving size indicated.) In addition, some products include other potentially (but not necessarily proven) stimulant contents, or substances that potentiate the stimulant action of caffeine, in addition to the caffeine itself: ephedrine, guarana, taurine, and ginseng, for example. Caffeinated beverage products also may contain high sugar content. The “energy” boost from the combination of stimulants and sugar is often followed by the kind of rebound effect previously mentioned: an extreme, precipitous drop in energy when the effects of these combined substances wear off.
While prevalence estimates for caffeine use disorder among the general population vary widely, it likely lies in the neighborhood of 9% (Meredith, Juliano, Hughes, & Griffiths, 2013). Diagnostic criteria for caffeine withdrawal syndrome also are described in the DSM-5 (Meredith et al., 2013):
- that caffeine has been consumed for a prolonged period
- 3 or more symptoms within 24 hours following an abrupt cessation (or significant reduction) in caffeine consumption, including headache, fatigue/drowsiness, depressed mood or irritability, difficulty with concentration, and nausea/vomiting or muscle pain/stiffness
- these symptoms cause significant functional impairment (social, occupational, or other important areas)
- these symptoms are not associated with another condition, mental disorder, intoxication, or withdrawal from other substances.
Tea. “Tea” is derived from the leaves of tea plants (camellia sinensis) and sold as black (e.g., Early Grey, English breakfast), oolong, green, or white tea. Like other botanically derived substances, caffeine content varies as a function of growing conditions, age of the leaves (more oxidation means more caffeine), handling/storage, and how it is brewed. Matcha is powdered green tea and has levels of caffeine greater than what is present in a brewed green tea preparation: the entire leaf is consumed rather than discarded after producing the infusion made from the leaves (https://www.oola.com/life-in-flavor/2308311/which-tea-has-the-most-caffeine/). Decaffeinated tea is one of previously mentioned types which have undergone one of several processes (carbon dioxide, ethyl acetate, methylene chloride, water processing) to remove as much caffeine as possible (https://www.cupandleaf.com/blog/pros-and-cons-of-drinking-decaf-tea). Caffeine-free herbal “teas” may be completely caffeine free because they do not actually contain any tea.
 Coffee. Coffee is produced from the beans of coffee plants (coffea). The caffeine content in a coffee beverage is highly dependent on the type of coffee, different coffee brands, and how it is brewed. For example, cold brew coffee generally contains a somewhat higher caffeine content than typically brewed coffee, and the same amount of espresso contains much more caffeine (https://www.medicalnewstoday.com/articles/324986#caffeine-content-by-coffee-type) See the comparison chart below for more specifics.
Coffee. Coffee is produced from the beans of coffee plants (coffea). The caffeine content in a coffee beverage is highly dependent on the type of coffee, different coffee brands, and how it is brewed. For example, cold brew coffee generally contains a somewhat higher caffeine content than typically brewed coffee, and the same amount of espresso contains much more caffeine (https://www.medicalnewstoday.com/articles/324986#caffeine-content-by-coffee-type) See the comparison chart below for more specifics.
 Chocolate. Caffeine is present in the beans of cacao trees (theobroma cacao) from which chocolate is produced. (Note that chocolate producing cacao plants and cocaine producing coca plants are very different types.) In general, the darker the chocolate, the greater its caffeine content (https://greatist.com/eat/does-chocolate-have-caffeine#1). “White chocolate” is produced from cocoa butter in the cocoa bean rather than from chocolate solids (cacao nibs), hence it does not have the dark brown color of the bean and also does not have caffeine. As you can see from the comparison chart below, the amount of caffeine in chocolate is considerably less than in most of the caffeinated beverages but the amount consumed is dependent on serving size.
Chocolate. Caffeine is present in the beans of cacao trees (theobroma cacao) from which chocolate is produced. (Note that chocolate producing cacao plants and cocaine producing coca plants are very different types.) In general, the darker the chocolate, the greater its caffeine content (https://greatist.com/eat/does-chocolate-have-caffeine#1). “White chocolate” is produced from cocoa butter in the cocoa bean rather than from chocolate solids (cacao nibs), hence it does not have the dark brown color of the bean and also does not have caffeine. As you can see from the comparison chart below, the amount of caffeine in chocolate is considerably less than in most of the caffeinated beverages but the amount consumed is dependent on serving size.
 Soft drinks and energy drinks. A tremendous amount of caffeine consumption occurs with certain types of soft drinks, including the diverse class of “energy drinks” and “energy shots” currently on the market. Energy drinks are sold in container sizes similar to those of soft drinks, whereas energy shots are concentrated liquids sold in small containers (about 2 ounces). “Next to multivitamins, energy drinks are the most popular dietary supplement consumed by American teens and young adults” (https://nccih.nih.gov/health/energy-drinks). You may recall from our module focused on alcohol the potential problems associated with the practice of mixing alcohol and energy drinks—the stimulant of the energy drink off-setting some of the sedative effects of the alcohol, such that individuals may drink more in a short period of time than is safe (i.e., engage in high intensity binge drinking). The caffeine content in different products varies widely (see comparison chart below) and, adding to the confusion, the contents listing may refer to single serving sizes when the packaging encourages 2 or more servings be consumed at once.
Soft drinks and energy drinks. A tremendous amount of caffeine consumption occurs with certain types of soft drinks, including the diverse class of “energy drinks” and “energy shots” currently on the market. Energy drinks are sold in container sizes similar to those of soft drinks, whereas energy shots are concentrated liquids sold in small containers (about 2 ounces). “Next to multivitamins, energy drinks are the most popular dietary supplement consumed by American teens and young adults” (https://nccih.nih.gov/health/energy-drinks). You may recall from our module focused on alcohol the potential problems associated with the practice of mixing alcohol and energy drinks—the stimulant of the energy drink off-setting some of the sedative effects of the alcohol, such that individuals may drink more in a short period of time than is safe (i.e., engage in high intensity binge drinking). The caffeine content in different products varies widely (see comparison chart below) and, adding to the confusion, the contents listing may refer to single serving sizes when the packaging encourages 2 or more servings be consumed at once.
 Other forms of caffeine. Caffeine has been made available in liquid, powder, and gum forms, and many of these products have received significant warning from the U.S. Food and Drug Administration because of their potential for misuse. Products with very high caffeine content can lead to overdose, which can be fatal just as overdose with any other stimulant substance. Their caffeine content is presented in the comparison table below.
Other forms of caffeine. Caffeine has been made available in liquid, powder, and gum forms, and many of these products have received significant warning from the U.S. Food and Drug Administration because of their potential for misuse. Products with very high caffeine content can lead to overdose, which can be fatal just as overdose with any other stimulant substance. Their caffeine content is presented in the comparison table below.
Nicotine.
 Leaves of the tobacco plant (nicotiana tabacum) also can produce a stimulant effect when chewed, “sniffed,” or smoked. Smoking tobacco or nicotine-containing products include cigarettes, cigars, pipe, hookah, and e-cigarettes (vaping). As of May 2016, federal regulations on tobacco products were extended to include all these forms; as of December 2019, regulations concerning the sale of tobacco products raised the minimum age from 18 to 21 years; and, as of January 2020, the Food and Drug Administration issued policy regarding the sale of flavored vaping cartridges as a means of reducing their attractiveness to minors (NIDA, 2020)a.
Leaves of the tobacco plant (nicotiana tabacum) also can produce a stimulant effect when chewed, “sniffed,” or smoked. Smoking tobacco or nicotine-containing products include cigarettes, cigars, pipe, hookah, and e-cigarettes (vaping). As of May 2016, federal regulations on tobacco products were extended to include all these forms; as of December 2019, regulations concerning the sale of tobacco products raised the minimum age from 18 to 21 years; and, as of January 2020, the Food and Drug Administration issued policy regarding the sale of flavored vaping cartridges as a means of reducing their attractiveness to minors (NIDA, 2020)a.
Nicotine is the primary psychoactive substance involved, however there are more than 7,000 chemicals produced in tobacco smoke, many of which are known to cause cancer (https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco/cessation-fact-sheet). These include acetaldehyde (we learned about this one in the focus on alcohol module), arsenic, benzene, formaldehyde, and vinyl chloride, and several toxic metals/elements such as polonium-210, cadmium, chromium, and beryllium).
Nicotine has a relatively high addictive potential, being quickly absorbed, causing the release of epinephrine and activating the brain’s dopamine reward circuits (NIDA, 2020a). Tobacco smoke contributes to a host of physical health problems/diseases: lung, oral, and other cancers; chronic bronchitis and emphysema; heart disease, heart attack, and stroke; Type 2 diabetes; cataracts; and poor pregnancy outcomes that include miscarriage, stillbirth, premature birth, and low birth weight, as well as learning and behavioral problems (NIDA, 2020a). Chronic obstructive pulmonary disease (COPD) is an additional health risk associated with smoking (https://medlineplus.gov/ency/patientinstructions/000696.htm). In the immediate short-term, nicotine has the familiar effects of the stimulant class of substances: fast (and sometimes irregular) heartrate, elevated blood pressure, appetite suppression, and increased focus of attention. Withdrawal symptoms include difficulty with paying attention, irritability, disordered sleep, increased appetite, and intense nicotine craving (NIDA, 2020a). Nicotine addiction related to use of tobacco products is discussed in the DSM-5 as a tobacco-use disorder. Many smoking cessation aids currently available offer a gradual withdrawal experience: gums, patches, and prescription medications (Portelli, Munjal, & Leggio, 2020).
The Surgeon General’s Report on Smoking Cessation, released in January 2020, offers evidence that smoking cessation is beneficial at any age, improves health status and enhances quality of life. It also reduces the risk of premature death and can add as much as a decade to life expectancy (NIDA, 2020).
Smoking cigarettes is more than an individual, personal choice: the respiratory and cardiac health of others is affected by exposure to second-hand smoke. Infants and young children are also affected by exposure to third-hand smoke: the smoke residue that accumulates on hard and soft surfaces (e.g., carpeting, furniture, car seats) in areas where someone has been smoking (Begun, Barnhart, Gregoire, & Shepherd, 2014).

E-cigarettes.
Electronic or e-cigarettes are devices intended to administer nicotine (and possibly other chemicals/substances) through inhaled vapor—similar to traditional “combustible” cigarette smoking but without actual combustion and tobacco leaves being involved. “There is substantial evidence that e-cigarette use results in symptoms of dependence on e-cigarettes,” and moderate evidence that the risk and severity of such dependence is lower than for combustible tobacco cigarettes (NAS, 2018). The term “vaping” is related to e-cigarettes also being named e-vaporizers. Some common nicknames for the devices are e-cigs, e-hookahs, hookah pens, vapes, vape pens, and mods (NIDA, 2020b).
Originally marketed as a tool to facilitate smoking cessation, these devices still deliver the addictive substance (nicotine) in amounts equivalent to that delivered from traditional combustible cigarettes (NAS, 2018). Hence, an individual who begins using e-cigarettes (vaping) remains at high risk of developing a nicotine addiction without ever having used a tobacco product. While they do deliver fewer and lower levels of many toxic substances compared to combustible tobacco cigarette smoke, most e-cigarettes do emit potentially toxic substances, although the amount and type is variable (NAS, 2018). The evidence surrounding the potential for increased cancer risk with e-cigarette use (compared to no cigarette use) is just beginning to emerge, but is not yet conclusive (NAS, 2018). An additional concern is raised by results of studies showing that use of e-cigarettes in early adolescence was associated with transitioning to established cigarette use within the near future (Chaffee, Watkins, & Glantz, 2018; Levanthal et al., 2015; NAS, 2018).
 Despite how they are marketed, e-cigarettes are not approved by the FDA for treatment of nicotine/tobacco addiction because strong evidence supporting use for this purpose is lacking; other approved alternatives are backed by evidence (NIDA, 2020b; Portelli, Munjal, & Leggio, 2020). In terms of a harm reduction strategy (compared to combustible cigarette smoking), adults’ use of e-cigarettes may reduce their exposure to some toxins and carcinogenic substances if used exclusively and not alternated with cigarette use (NAS, 2018).
Despite how they are marketed, e-cigarettes are not approved by the FDA for treatment of nicotine/tobacco addiction because strong evidence supporting use for this purpose is lacking; other approved alternatives are backed by evidence (NIDA, 2020b; Portelli, Munjal, & Leggio, 2020). In terms of a harm reduction strategy (compared to combustible cigarette smoking), adults’ use of e-cigarettes may reduce their exposure to some toxins and carcinogenic substances if used exclusively and not alternated with cigarette use (NAS, 2018).
In addition, there exist significant concerns regarding the safety of these devices. In addition to the health concerns previously noted, the devices themselves pose risks. “There is conclusive evidence that e-cigarette devices can explode and cause burns and projectile injuries” (NAS, 2018). As in the case of second-hand (and possibly third-hand) smoke exposure from traditional combustible cigarettes, there exists conclusive evidence that e-cigarette use causes increased concentrations of airborne particulate matter and nicotine in indoor environments and limited evidence of contaminants on indoor surfaces (NAS, 2018). The harm from second-hand e-cigarette exposure is likely less than the harm associated with second-hand cigarette smoke exposure (NAS, 2018).

Exposure to the nicotine-containing liquids used to fill e-cigarette reservoirs can cause significant health problems if it comes into contact with a person’s eyes or skin, or if it is consumed by drinking or injection (NAS, 2018). The most common types of nicotine overdose fatalities occur when young children consume these liquids (NIDA, 2020).
Finally, the FDA and the Centers for Disease Control and Prevention (CDC) have posted public alerts concerning clusters of vaping deaths attributed to poor quality vaping devices or nicotine liquid formulations, and especially to vaping liquids containing other substances such as THC (the psychoactive ingredient in cannabis) or vitamin E acetate (used as a thickening agent). As of February 4, 2020, a total of 2,758 hospitalizations or deaths were reported to the CDC related to e-cigarette or vaping associated lung injury (EVALI); rates are gradually declining following a sharp increase in August and September of 2019 (CDC, 2020).

STOP & THINK
Visit the caffeine informer website (https://www.caffeineinformer.com/the-caffeine-database) and calculate the caffeine content in the serving sizes of products you enjoy consuming. Consider the following questions:
- What effects do you think this might have on your health and behavior (positive and/or negative)?
- Do you think that a person might develop tolerance to the products you enjoy with a prolonged period of regular use at the levels you like to use them?
- Do you think a person might develop withdrawal symptoms if abruptly stopping the use of these products following a prolonged period of regular use at the levels you like to use them?
- What might be good ways for a person to change the “habit” of using these products?
