Chapter 15 – Flee Wikkyd Heires

Pick up a flea and hold it to the light. You can almost see right through it. With its extreme lateral compression, it seems determined to operate in two dimensions. Denuded of wings, it uses its robust saltatorial (jumping) hind legs to vault up to 200 times its own body length (Figure 15.1). It is a curious creature, almost comical in a sense but also deadly serious in ways that mankind is not likely to forget. Indeed, we must not forget. The amount of creative power we have harnessed to describe and study the impact of this beast on our world is epic. Here begins a tale, the likes of which our species has rarely seen. Imagine what life would be like to leave your loved ones in the morning and find them all deceased by dinner. Imagine what would happen to your faith in the ordinary institutions we use to make sense of the world and to guard against its chaos when they prove completely and utterly feckless in meeting the challenge of the flea. Religion won’t save you. Medicine is incompetent. Government officials and policy makers have left town hoping to go to a place where the flea won’t find them. You are on your own to face one of the most devastating challenges known to mankind. All of this because of a little insect so small you can barely see it. This is the story of the flea and the apocalyptic terror it brought to mankind. This is the story of the Black Death, the medieval plague that killed half of the population of Europe in two and a half years in the 14th century.
In fairness, not all the blame goes to the flea. This is a really a story about the complex ecological relationship between four species, one of which is mankind. The players in this historical nightmare include the causal agent (or pathogen), the bacterium, Yersinia pestis. The primary or intended host is the Oriental rat flea, Xenopsylla cheopsis. Both male and female rat fleas take blood meals for needed nutrition, a requirement that brings a third species into the mix, namely the rat. As with other insect-vectored diseases, the rats become infected when they are bitten by infected fleas, thus passing the pathogen along when the flea chooses the next rat to bite. In this sense, rats represent the first victim of the bubonic plague. And if hygienic practices had been strict, the cycle might end there. But in medieval times and, indeed, in some places today, rats and humans live in close proximity. The fleas that live on rats can also bite humans, spreading inoculum to human victims as well as to other rats. Humans are, thus, the fourth albeit unintended player in this saga.
Naming the Catastrophe
The plague that occurred in Europe in the 14th century is typically referred to as The Black Death. However, this descriptor did not arise in the 14th century. So, where did the phrase come from? Author and historian, Philip Zeigler (The Black Death, 1969) has pointed out how baffled medieval people were by the pandemic plague. According to Zeigler, “it was totally incomprehensible.” Further, Zeigler argued that “Medieval man was equipped with nothing in the way of defenses against the devastation of the plague. That is to say, medieval humans lacked social, medical, and psychological means both to understand what was happening and to guard against it. The plague, in other words, rent the fabric of society, overwhelming the coping skills of a population that was not equipped for the staggering death toll and the abject misery that the plague brought.”
As the plague has been exhaustively studied in our time and throughout history, it is surprising that no one has yet explained the origin of the phrase “The Black Death.” Ziegler noted that most scholars assumed that the phrase came from the ghastly appearance of flesh in victims of septicemic plague when blood moves outside the capillaries and clots, giving the skin a blackish appearance. Since it takes place largely in the extremities (toes and fingers) it is referred to as acral necrosis or acral gangrene.
Ziegler points out that acral necrosis, although hideous and scary is not likely to have been the source of the phrase “The Black Death,” since 80% of the plague victims had the bubonic form (as opposed to septicemic), which does not involve acral necrosis. In support of that point, no one in the 14th century referred to the pandemic plague as The Black Death. In fact, the phrase was not used as a reference to the plague until the 18th century.
Other references to The Black Death have appeared periodically in the literature. For instance, the phrase Swarta Doden (black death) was used in Sweden in 1555, and the phrase Sorted Dod found its way into a Danish periodical in 1605. An English cleric, Cardinal Gasquet, said that The Black Death received its name in 1665 in an effort to distinguish it from the Great Plague, the name given to the plague that erupted in London from 1664-1666, killing over 100,000 Londoners.
Some other more fanciful ideas were advanced about the origin of The Black Death as well: one chronicler suggested it came from the siting of a black comet before the plague arrived in Europe, or that the term Black was a reference to the black mood of the people as the mortality mounted. Other possibilities were metaphorical. For instance, the plague was depicted as a man on a black horse or as a black giant striding across the landscape. But, again, lack of usage during the medieval plague suggests that these are not the reasons.
So, where did the phrase, “The Black Death” really come from? Zeigler says that it is an overliteral translation of a Latin phrase—pestis atra or atra mors. For the non-Latin scholars among you, in medieval times, the word atra connoted the idea that something was dreadful or terrible as well as black. Pestis, of course, means pest. Finally, mors means death.
Thus, we have the black (dreadful) pest and the black (dreadful) death as two possible source phrases. Either way, the modern mind would not consider any other phrase sufficient to capture the horror to call it anything else but The Black Death. The phrase “The Black Death,” is thus, cemented into our minds as synonymous with the medieval plague.
Describing the Players
The Bacterium: Yersinia pestis
The protagonist in this saga is the plague bacterium, Yersinia pestis. It is a gram-negative obligate parasite that cannot live outside the host. In that sense, it is a fragile organism whose existence depends heavily on being transmitted in a way that keeps the bacterial cell sheltered from the environment. Sadly, there are many species of the genus Yersinia, many of which are disease-causing. The level of virulence varies with the species and the strain. While the other forms of Yersinia besides Y. pestis can cause illness, the conditions produced by these close cousins of the plague bacterium generally involve some form of gastroenteritis (a stomach ache).
Using genetic techniques, we know that the plague-causing bacterium evolved from a related species, Yersinia pseudotuberculosis, around 20,000 years ago. There is a third species of Yersinia, Y. entercoliticus, which like Y. pseudotuberculosis is spread via the fecal/oral route of transmission. This means that exposure takes place when a mammal, including humans, comes into contact with infected feces that are subsequently ingested. Both Y. pseudotuberculosis and Y. entercoliticus produce a fairly mild gastroenteritis as their main effect in mammals. The fact that a relatively harmless bacterium that is spread via the fecal/oral route gave rise to the much more virulent form, Y. pestis, that is spread via the much more specialized blood-borne route, and in a comparatively short period of time is a matter of some concern. The genetic plasticity of Yersinia appears as though it may be quite high, suggesting that other highly virulent forms with possible activity in humans may arise. A possible benefit to the high malleability of the Y. pestis genome is that it appears to lose genes from its genome from time to time. It is likely that this loss is the reason why plague in Europe after The Black Death of the 14th century became less virulent with each reappearance.
If we confine our attention to the species Y. pestis, we currently recognize three biotypes: Antiqua, Medievalis and Orientalis, each of which was associated with a major plague epidemic in humans. We don’t know much about genetic distinctions among the different types, although it would be useful to know if there are such differences and what impact they had, if any, on virulence. As previously noted, it seems to be the case that as the medieval plague recurred in Europe after the 14th century, it was less lethal, but it is not known whether that is due to a genetic change or some other factor.
Like a typical bacterium, the plague bacterium has a well-known capacity for developing and spreading resistance to antibiotics in its progeny. One of the major ways Y. pestis adapts to changing conditions is by using bacterial plasmids to exchange genes. Genes that are critically important for bacterial survival are often packed into DNA that is contained in plasmids. During reproduction, bacteria can form a “conjugation bridge” between two bacterial cells. The bacteria can then exchange plasmids, and the DNA they contain, between cells. This is a very rapid way of disseminating genes between individual bacterial cells. We know that Y. pestis has at least two plasmid-borne genes that are responsible for the virulence of the disease. One encodes for a plasminogen activator; the other is a murine toxin that encodes a high level of lethality for rats. While these two genes may not be of concern to humans, the likelihood that the plague bacterium could develop resistance to antibiotics, the main treatment for plague in modern times, and then spread the trait via plasmid transfer is both a realistic prospect and one that is very scary. This is yet another reason to avoid the overuse of antibiotics. f nothing else, we need to appreciate that the plague bacterium is ingenious in its ability to spread the suffering around.
The Flea: Xenopsylla cheopsis
The flea in question is a pulicid (Family Pulicidae) and most often, we will be concerned about the rat flea, Xenopsylla cheopsis. However, there are other fleas that might have potentially been involved in the plague. The human flea (yes, there is one!), Pulex irritans is capable of transmitting plague as is the human body louse. However, X. cheopsis gets most of the credit for The Black Death. One reason for this is that a critical aspect of rat flea’s biology made the plague much worse than it might otherwise have been. As the plague bacterium multiples inside infected fleas, the bacterial cells accumulate in the narrow passageway in the gut, called the proventriculus, of the flea. The accumulation of cells there blocks blood from getting into the stomach of the flea where it can be digested and used nutritionally. Since, with a blocked proventriculus, the blood meal never gets to the stomach, the flea begins to starve. And, of course, the flea’s response to being hungry is to find more mammalian victims to feed on, thus, passing the plague along as it goes. This will be discussed in greater detail later in the chapter, as it is, perhaps, the most critical element in the infectivity of the plague.
As with other blood-feeding insects, fleas of many species have cultivated a variety of adaptations to ensure their ability to draw a blood meal from an unwilling mammalian host. These include specialized mouthparts for penetrating skin and withdrawing blood. Fleas also use CO2 expired from the host as a means of locating its intended victim. Of course, many blood-feeding arthropods have these adaptations, as mentioned in Chapter 12. However, some other adaptions are specific to the flea. These include the loss of its wings, ostensibly an adaptation to prevent its wings from being caught up on the hair of the host, and the incredible jumping power of the fleas’ hind legs which, as previously noted, can catapult a flea distance 200 its body length. Without wings, this is the flea’s primary means of independent locomotion. Of course, fleas can hitch rides on their ambulatory hosts as well.
Other elements of the flea life cycle also enhance its ability to spread diseases of interest to humans. The preferred host of the Oriental rat flea is, as the name suggests, the rat. However, the rat flea will feed upon the blood of other species as well, including dogs, cats, and humans. This lack of a strict host preference, of course, was critical in spreading the plague to and among humans.
A variety of other characteristics of the rat flea also made it an efficient vector for infecting humans. For instance, a gravid female will lay her eggs in the bedding of the host. If you’re a rat, this means the material used to make a nest such as straw. If the flea is feeding upon humans, it generally means bedding material. Larvae will hatch from 1–10 days later depending on environmental conditions, such as temperature. The larval stages feed upon detritus left by the host in the nest or bedding and will then pupate. The pupal stage can last and remain viable for a considerable period of time (1–6 months). This allows the pupae to survive through difficult environmental conditions and allows them to wait for good conditions before completing their metamorphosis. Eventually, the adults will emerge and the female will take a blood meal so that she can produce eggs. Importantly, a flea can survive in its various forms for up to a year without taking a blood meal. This, of course means that considerable care has to be given to eliminating all life stages when trying to control flea-vectored diseases. n medieval times, there was no awareness that fleas were a culprit in the transmission of the plague and, therefore, there was no incentive to go to the trouble of trying to control them other than for the sheer irritation they cause. Even if that had stimulated interest in controlling fleas, hygienic practices were not well-developed compared to today’s standards and there would have been little ability to control fleas by cleaning up. The typical medieval peasant, after all, lived in a hovel with a dirt floor. Many had domiciles located close to barns or other areas where animals, including rats, would have been common. As a result, the major players cohabited, making the transmission of plague an event with a high probability.
Another critical factor that made the rat flea ideally suited for transmitting plague in a non-preferred host such as humans relates to adaptations that the flea had to assure good blood flow from the host to the flea. The flea gains access to host blood by penetrating the skin of the host and inserting its mouthparts into a capillary from which the flea pumps blood into its gut. However, a major problem with this feeding style is that once the skin is pierced, the clotting mechanisms rapidly kick in and the blood around the wound site begins to coagulate. This, of course, means that the ability of the flea to obtain a large blood meal, as is required for reproduction, will be limited. Fleas (like mosquitoes) have met this challenge by producing saliva that has anticoagulants in it to prevent the normal clotting that would take place. Since the flea is spitting saliva into the host, if that saliva is contaminated with plague bacteria, the host will be the recipient not only of an itchy bite, but a deadly pathogen as well.
As previously mentioned, even the flea—the primary host, is not spared the ravages of the plague. Figure 15.2 (click on link) shows the basic digestive system of an orthopteran insect. The proventriculus is a narrow passage way located between the crop and the midgut and is narrower than what comes before or after it. The cells of plague bacterium have the characteristic of being “sticky.” In the proventriculus of the flea, plague bacteria can stick to the walls. Because this is a narrow passage way, as the bacterial cells stick to the wall of the proventriculus, they occlude (block) the passage, eventually making it impossible for blood to flow through the proventriculus to its intended destination in the stomach where the blood would be digested (Figure 15.3 – click on link & open full text). The flea, thus, continues to bite because the food it ingests isn’t nourishing the flea. The continued biting spreads plague-contaminated blood and saliva to additional victims as the flea tries desperately to get a meal. We also know that only fleas with a blocked proventriculus transmit disease. This probably explains why the rat flea is critical to The Black Death. For reasons that we do not fully understand, the proventriculus of the rat flea is more likely to become blocked by plague bacteria than the proventriculus of other species of fleas. Thus, Xenopsylla cheopsis was probably a necessary predicate in creating the conditions that would bring about The Black Death. In other fleas, the proventriculus would not be blocked and those fleas would be less effective in spreading the pathogen.
The Rat: Rattus orientalis
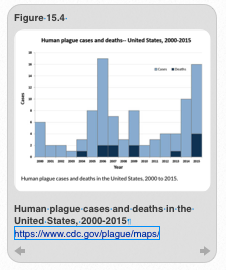
The preferred host of the rat flea is the rat. But the rat flea is also quite at home living with and using other rodents or non-rodents as a food source. In the United States, the plague bacterium occurs in nature, although it is primarily found in the southwestern U.S. A small number of cases (10–17) of plague occur in humans in the United States every year. In some years, the plague kills a very small number of people (Figure 15.4). Since plague is treatable with antibiotics, the victims can usually be saved if they are diagnosed and treated quickly. There is a slightly greater prevalence of plagues cases among men compared to women, which probably relates to the greater tendency of men to be involved in outdoor sports, such as hunting, which potentially brings them into contact with infected wildlife and fleas. In 2015, two plague fatalities occurred in the southwest. In all probability, the inoculum was transmitted from wild rodents such as prairie dogs to domestic animals such as cats and from cats to humans by the rat flea.
In modern times, the threat of plague is not due primarily to plague contracted from the bite of a plague-contaminated flea. Rather, the larger threat comes from use of plague as a biological weapon. As will be discussed in a later chapter, plague has been used several times as a mechanism for subduing human populations who are reckoned to be combatants. The first such incident of cultivating and weaponizing the plague bacterium is attributed to the Japanese during WWII. A secret branch of the Japanese army, Unit 731, produced plague-infested fleas, which they dropped over various populated parts of China, resulting in an outbreak of plague. However, the need to raise fleas, plague bacteria, and rats was onerous. As a result, when the United States took up the use of bubonic plague as a weapon of war, they avoided all of this by producing an aerosolized version of the bacterium that could be deployed into ambient air. Humans in the vicinity could inhale the aerosolized bacteria, which could then result in primary pneumonic plague.
The U.S. was less successful than the Soviets in developing plague as a biological weapon. The amount of plague produced by U.S. scientists was insufficient to make an effective weapon. However, the Soviets were reported to have produced enough to deploy as aerosolized weapons. In the United States, the plague program was suspended in 1970.
Returning to medieval times, the fact that rats were infected with plague bacterium and that, in medieval times, rats lived in close proximity to humans was enormously consequential to The Black Death. Rats, like humans, are killed by the plague. Fleas cannot suck blood from a dead rat. As a result, the death of the preferred host of the rat flea meant that the flea would search for a new blood source. Humans living in rat-infested houses, thus, became an acceptable alternative to the rat flea whose host preferences were never very strict to begin with.
The Fourth Player: Homo sapiens
Finally, the last players in our saga are humans. Here we have a fairly detailed understanding of transmission and virulence—at least in modern times. We know that humans can be exposed to plague via three routes:
1. The bite of an infected flea.
2. Aspiration of the sputum of people infected with the pneumonic form of the disease, which affords a direct route of the bacterium to lungs and the respiratory system.
3. Handling the carcasses of rodents with plague, and aspiration of saliva of persons with the plague (less-established, but possible routes of transmission).
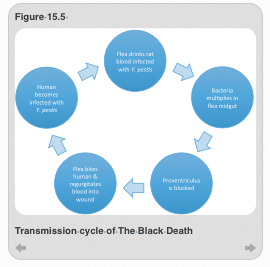
Of the three modes of transmission, the first, the bite of an infected flea, is the most critical because this is the step that wrests the plague bacterium from the world of the flea, which is the intended victim of the bacterium, and inserts it into the human world (Figure 15.5). Once infected, the plague bacterium will multiply inside the flea, resulting in a blocked proventriculus. This, of course, increases the infectivity of the flea by preventing it from ingesting the blood intended to nourish it and forcing it to continue biting in order to obtain the food it needs to sustain it. However, that will prove impossibly elusive with a blocked proventriculus, forcing the flea to keep biting in order to eat. Of course, the pathogen spreads every time the flea bites and reflexively regurgitates a small amount of the now plague-contaminated blood and saliva into each mammal bitten. Because the rat flea will opportunistically feed on whatever source of mammalian blood it can find, eventually the very hungry flea will choose a human victim and the plague takes root in humans. From that point on, the plague can continue to spread via additional flea bites, or through the inhalation of bloody sputum in the absence of fleas.
Forms of Plague: Modern Perspective
In modern times, we have a fairly sophisticated understanding of the symptoms of bubonic plague and the progression of the disease. Once inside the human body, the plague bacterium can invade multiple sites, leading to three different types of plague. In the first type, the bacterium will travel through the blood and invade the lymphatic system. Here, the bacterium will reproduce rapidly and result in the formation of nodules in the lymph nodes which are called buboes. The buboes fill with blood giving the lymph nodes an eerie black color. Generally, this is the first sign of plague—called bubonic from the presence of buboes. Bubonic plague cannot be transmitted from human to human in the absence of an infected flea.
In another type, plague bacteria circulating in the blood may also invade and reproduce in the lungs. In response, the lungs may begin to hemorrhage internally. Because this is all happening in the lungs, it is referred to as the so-called pneumonic form. And since this form began as bubonic plague and morphed into pneumonic plague, it is referred to as secondary pneumonic plague. It is particularly dangerous because every time the victim exhales, he can send plague bacteria or plague-ridden bloody sputum into the air where others may breathe it in. It is the major mode of transmitting plague in the absence of fleas. When plague is transmitted in this way (breathing in infected sputum), it is called the primary pneumonic form since it did not begin as bubonic.
Finally, plague bacteria may begin to multiple in the blood. The blood itself becomes contaminated with massive amounts of plague bacterium, resulting in a systemic infection of the blood, called septicemic plague, which is the most deadly of the three forms. A very small percentage of plague begins as the septicemic form and is, therefore, called primary septicemic form. In this case the bacterium enters the blood as the result of a contaminated flea and instead of lodging in the lymph nodes and becoming the bubonic form, it instead begins to replicate in the blood and become septicemic. There is no eruption of buboes and there is no direct transmission to other humans. This form of plague was no doubt very confusing to medieval physicians who would have been flummoxed by the lack of buboes. There is also a secondary septicemic form that begins as bubonic plague with presentation of buboes but then becomes septicemic as the bacteria begins to replicate in the blood. All forms of plague and their characteristics are summarized in Table 15.1.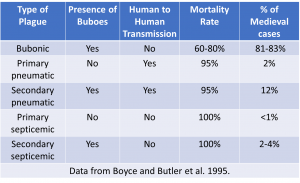
A classic progression of symptoms in the case of bubonic plague would begin with the appearance of buboes in the groin, neck, and armpits—the sites of the major lymph nodes. Swollen buboes may open up and ooze blood and pus. The buboes fill with pus and can increase to the size of an egg or an orange. Accompanying symptoms include fever, headache, joint pain, diarrhea, dehydration, and vomiting. The bubonic form was the most common form of plague during The Black Death, comprising about 81-83% of all plague cases. The mortality rate of this form ranged between 30–80% (depending on the academic source) with death coming 4–7 days after the onset of symptoms.
In some cases, the plague bacterium will invade and reproduce in lung tissue, resulting in pneumonic plague with symptoms appearing as fever and a cough with blood-tinged sputum. The skin may appear slightly blue due to lack of oxygen. This, of course, is truly frightening to behold. Other symptoms that may present with the pneumonic form of plague include a high fever, nausea, vomiting, and weakness. This form is considerably more dangerous, both for the victim—with a mortality rate of 90–95%, and for healthy people sharing the quarters who would now be exposed to airborne plague bacteria in the bloody sputum of the victim. This form of plague progresses quickly and may result in respiratory failure and shock within two days if untreated.
The remaining form, the septicemic form, was invariably fatal in medieval times with a mortality rate of 100%, and for which there seemed to be very little in the way of an incubation period. In addition to a high fever, this form is identifiable from discoloration of the extremities (toes and fingers), called acral necrosis or gangrene. The dark coloration is due to internal hemorrhaging and subsequent cell death. As it progresses, the nervous system is affected, resulting in a variety of strange behaviors, which can vary between stupor and a raging delirium. The latter may include slurred speech, twisted facial expressions, and strange body movements. Ultimately, the victim goes into a coma followed by cardiac arrest. From start to finish, septicemic plague may cause death in less than a day. It is quite a painful and ghastly, albeit comparatively quick, way to die.
Forms of Plague: Medieval Perspective
Medieval physicians were baffled by the plague for several reasons. First, because of the existence of three forms of the disease (bubonic, pneumonic, and septicemic), the symptoms of the disease and prognosis varied widely. Physicians did not agree that they were dealing with a single illness. Second, the 14th century took place four hundred years before the Germ Theory of Disease cemented our understanding of the role of microscopic pathogens in causing disease. As a consequence, medieval physicians did not understand that the plague represented a single pathogen capable of manifesting itself in different symptomologies. Third, medicine at the time of The Black Death was still an enterprise that hewed to the Galenic tradition of understanding of how disease was created in the body and, therefore, how disease should be treated. Given all of this, it is miraculous that were able to do anything productive to combat the plague.
In medieval times, there was much argument about whether the appearance of buboes portended imminent death. It is important because failure to adhere to find the eruption of buboes has been one cause for questioning whether bubonic plague or some other pathogen was responsible for the chaos we associate with the 14th century. On its surface, the notion that the appearance of buboes meant immediate death is false on at least two counts. First, the mortality rate for the bubonic form was generally somewhere between 30–80 percent (again, depending on source). This means that 20–70 percent of people stricken with bubonic plague recovered and did not die of the plague. Second, there are many reports of people lasting for many days, and sometimes longer, after the appearance of buboes. It is true, in contrast, that people who contracted pneumonic plague died more quickly, typically 1–2 days after the onset of symptoms, and those who were unlucky enough to contract septicemic plague may have died within hours. In the case of primary septicemic plague, there wasn’t enough time for the buboes to erupt.
Another important factor is that medieval physicians were not adept at separating the different types of plague and, therefore, were mystified by the different symptoms and the variable progression of the disease. One symptom that did seem to portend lethality, however, was coughing up blood. Those folks did not typically recover and would die shortly after the appearance of symptoms. As previously noted, this is also the form that can be spread in the absence of rats and fleas, thus confounding an understanding the cause(s) of the disease.
Among the medieval chroniclers, there were some very graphic descriptions of how devastating plague could be. Geoffrey the Baker, for instance, remarked that apparently healthy people might go to bed at night and be dead of plague by morning. Similarly, Simon of Covino wrote about healthy clerics who would go to visit a plague patient, contract the disease while visiting and die before the sick person they had come to see expired. When these dramatic, very rapid deaths were contrasted with the lingering bubonic form of the plague, it is no wonder that physicians had difficulty parsing out the three different types. What everyone internalized is that the appearance of plague meant disaster and everyone was terrified that plague meant instant death. Thus, Ziegler’s observation about the bewilderment of medieval people makes abundant sense.
Of course, critical to understanding the plague and taking appropriate preventative measures, is to know how the plague is transmitted. In medieval times, this knowledge simply didn’t exist. Indeed, medieval theories about transmission of the plague were confused by the reality that there were different forms of the plague, and as we now know, different modes of transmission. Since understanding transmission could assist in preventing the spread of the disease, it was important to get a handle on this issue. In Medieval times, there were two basic ideas about how plague was transmitted: one was that a sick person could transmit it directly to a well person. With the exception of pneumonic plague, that is probably not true. The other idea is that the plague-causing element was circulating in the air like a poison cloud, or miasma as it was generally called. Both prospective modes of transmission had the benefit of explaining the sudden sickening of large numbers of people. This was an idea already well-ingrained in the medieval mind and which seemed to have an evidentiary basis.
One pattern noticed by medieval physicians was that a zone of mortality of plague would develop and then stop as the zone of mortality shifted somewhere else. This was taken as evidence against the person-to-person transmission. Why would plague transmission erupt and then stop all of a sudden? This seemed to favor of the miasma theory. A toxic cloud or miasma could invade an area quickly in response to some invisible and unknown force and then leave and go to another area. This could explain why plague mortality traveled. Thus, the idea that the air was corrupt and that its movement spread the plague gained currency. This may also have been the logic behind the construction of masks, employed by physicians, to filter out the toxic air and, thus avoid the plague, even when liberally exposed to plague.
Because the miasma theory was favored, there was much discussion about the nature of the toxic plague cloud. One issue to resolve was whether the miasma, once formed, was permanent. Some, such as the philosopher Ibn Shatimah said “ yes.” He believed that the physical nature of the air was fundamentally changed by the putrefaction of the plague and that, henceforth, no living thing could survive by breathing the tainted air. It was more common, however, to believe that the poisoning of the air was temporary. This seems to comport better with the idea of a portable toxic cloud as well.
Of course, in addition to the standard understanding of how the air was poisoned, there were some fringe theories as well. For instance, Alfonso of Cordova argued that celestial movement of the planets caused poisoning of the air while others argued tectonic movement of the earth, e.g., through earthquakes, released toxic air that had been safely stored underground and, once released, caused the plague.
There was also a sort of accommodationist school of thought that tried to join both the miasmatic, toxic cloud idea with the person-to-person transmission scenario. Interestingly, there was some objection to the person-to-person modality on biblical grounds. But for the truly observant, the fact that apparently healthy people contracted plague while visiting the sick was too strong to ignore. Thus, a convenient hybrid mechanism emerged that had the benefit of explaining person-to-person transmission. This idea was that sick persons were the source of the miasma or toxic cloud. Like modern humans, there was always someone to take a somewhat plausible idea to a ridiculous extreme. In this case, frightened people argued that no miasma from the sick person was required. Rather, a mere look from the sick person could do the trick. The reality was, however, average people were mostly concerned with surviving the crisis and were much less concerned about the mechanics of how it was spread. The available evidence led many to conclude that isolation was the best solution. Hence the prescription to “Flee those Wikkyd Heires” seems remarkably prescient.
Where did the Plague Begin and how did it get to Europe?
Medieval people were forced to slog through life without knowing precisely how or why the plague came among them. But, we are able to make sense of that question from a modern perspective.
The wave of death followed trade routes that originated in Asia. First appearing in port cities in the Mediterranean in 1346, successive appearances of plague moved north and inland as the plague spread. Over a three-year period, the plague touched most of Europe.
Most sources argue that the plague came from Asia following the silk trade routes. However, that is not a very nuanced view. China is often identified as the source of the medieval plague—an idea fueled in part by the reality that a lot of calamitous things were happening in China during the 14th century. For instance, a massive drought and attendant famine raged in China; an earthquake in the mountains of Ki-Ming-Chan killed 5 million people and hordes of locusts depleted the food supply in Canton. While these were devastating events, they paled compared to what was to come, specifically the advance of the plague around the globe.
In modern times, a Russian archeologist named Chwolson, working near Lake Issyk-Koul in Central Asia found abnormally high death rates in Central Asia, a place where plague is known to be endemic, in 1338 and 1339. Gravestones in the area ascribe the deaths to plague. Thus, Central Asia is probably the location where the medieval plague incubated. It is likely that the activities of the Mongols who ruled much of China for 150 years were critical in moving the plague bacterium across the Mongolian steppes from China across India and then from the Middle East to Europe. The spread of plague was likely exacerbated by the militaristic activities of the Mongols. Once an enemy was slain, the bodies would be pillaged for furs and blankets. If those items were laden with fleas, the Mongols may have unwittingly acquired a deadly disease, which they proceeded to spread as trade routes expanded.
Among the things the Mongols did was to open up trade routes through Russia and India which eventually reached the Middle East and the city of Caffa as trade spread to the west via overland trades routes. Historical records suggest that the progression of plague from Mongol strongholds in China to Caffa took approximately nine years. Modern epidemiologist suggest that this rate of spread is roughly what one would expect for a disease with the etiology of the plague and the reality that travel was limited and slow.
As commerce extended from Asia to the Middle East, the plague followed. But, at Caffa, the mode of dispersal changed. Up to that point, the route by which the silk and spice trade spread from China to the Middle East involved the use of overland routes of travel. At Caffa, that modality changed to a seafaring method of travel as trade extended to Europe. It is at this point that the most common narrative about how the plague infected Europe takes over.
The typical story adduced to explain the entry of plague into Europe is that it hitched a ride on ships carrying silk, pelts for trade, and spices. There are a variety of chronicles from this time from which the march of the plague can be deduced. However, the accuracy of the authors is always a question. Even with these difficulties, it is possible to outline a possible shipping route in which the plague was passed from Asia to Europe.
Regardless of whether Central Asia or India was the original source of the plague, it was probably offloaded in the city of Caffa in what is now Turkey, according to a claim made by Gabriel de Mussis. De Mussis stated that the plague appeared in Caffa in 1346. At that time, the Mongols were interested in capturing a fort at Caffa, which had been fortified for trade, in anticipation of further extending trade routes. The Mongols were aware that they were being blamed for the arrival of the plague and wanted to deflect blame onto the Christians. The Mongols chased the Christians to the fort at Caffa. While sitting outside the city, waiting for a chance to attack, the Mongols became sick with the plague and were too weak to mount an attack.
Thus thwarted, the Mongols vowed not to let the opportunity go to waste. They catapulted plague-ridden corpses over the ramparts hoping to infect the Christians. This had the desired effect of sickening some within the fortified city. In order to escape the sickness, a large number of inhabitants decided to flee, taking the plague with them. The preferred route of exodus was to take ships to the Mediterranean.
The plague, thus, spread to Messina, a port city on the island of Sicily, which routinely received ships with goods for trade. Now ships were arriving with people suffering from a mystery illness. The people aboard the ships from Caffa were described as “dying at their oars” when they reached the various port cities. Inhabitants began to refuse to board incoming ships, leaving the goods to rot in the harbor. While this may not represent the first introduction of plague outside Asia, it set a pattern that would be repeated many times. And now plague was ready to spread across the European landscape.
From Sicily, it was only a short distance to the Italian mainland. Plague began to appear on ships pulling into port cities such as Venice. The arrival of the European plague, which began in roughly 1347, took two distinct trajectories once it took root. Plague continued to spread via merchant vessels that pulled into port cities. Once in port, plague could be spread by sick people leaving the ship and entering the cities to offload goods. Similarly, plague-carrying rodents and fleas may have left the ships on which they arrived and continued to spread the contagion around city. Indeed, fleas living on pelts in the hold of a ship would have access to dander on the pelt as a food source but not to blood. As a consequence, the fleas would have been very hungry by the time the ships docked and would have been actively looking for a source of blood. Second, once inhabitants of port cities realized that they were being exposed to a disease that was coming in from ships, they began to move inland and north to outrun the plague. As the local inhabitants had already been exposed to the plague inoculum, this simply accelerated the spread of the plague to land-locked cities. As the plague ran its course in Europe, a successive series of plague returned time and again in cities not yet recovered from previous rounds of plague.
Over a four year period, the bubonic plague claimed from one-third to one-half the population in Europe. There was considerable variation in susceptibility and virulence as the plague marched across Europe. In Italy, infection rates were as high as 80% while in England and Germany, it was closer to 20%. Similarly, death rates from plague in the Middle East were lower than in Europe, possibly a result of prior exposure. Interestingly, the virulence of the plague was reduced with each subsequent introduction. It was not until the 19th century, however, that Europe was plague-free.
The assumption made about the plague in Europe has always been that merchants brought plague from the China to European ports, after which some rodent, in which the bacterium found a congenial home, became the place where plague was maintained in the wild. In other words, there was a single (or limited) introduction of the plague from the East to Europe, after which, a wild reservoir of plague was created in Europe.
Recent evidence suggests that this is not true. In a recent paper by Schmid et al. (2014), the researchers investigated climate fluctuations that preceded plague outbreaks to locate plague reservoirs in nature. The research produced a data set of 7,711 plague outbreaks with accompanying climatic conditions derived from tree-ring records from both European and Asian sites. The evidence from the study suggest that rather than the establishment of a plague reservoir in Europe, the plague recurred in Europe as a result of periodic reintroduction of the plague from Asian rodent plague reservoirs. The climatic data show the prevalence of plague in great gerbils in parts of Central Asia such as Kazakhstan is correlated with warm springs and wet summers as determined from tree rings. The latter also correlates with high densities of gerbils and fleas, which can happen on a broad geographic scale, thus perpetuating the spread of plague. When climatic conditions favorable to gerbils decline, the transmission of plague is exacerbated because the number of fleas per gerbil will increase, making plague transmission more likely, and the fleas will seek alternative hosts which spreads the pathogen to additional species, including humans. In Europe, climatic conditions favoring high rodent populations and lots of fleas are confined to a narrow area in Europe near the Caspian Sea making it more unlikely that there is a permanent reservoir of plague bacteria in Europe outside of this narrow geographic band.
The misery caused by the plague was recorded everywhere, certainly in the books and periodicals which carried particular meaning to society. It is perhaps not surprising then that the plague would be memorialized with a miniature painting in the Toggenburg Bible (Figure 15.6). While desperately ill parishioners die in the foreground, a hapless priest scatters magical dust in the background hoping to mitigate the plague.
Writers of the time of the plague actively chronicled the plague-induced carnage. A quote from “The Plague in Sienna: An Italian Chronicle” by Agnolo di Tura captures the horror—“They died by the hundreds, both day and night, and all were thrown in ditches covered with earth. And as soon as those ditches were filled, more were dug. And I, Agnolo di Tura, buried my five children with my own hands. And so many died that all believed it was the end of the world.”
And so it was for so many in 14th century Europe. None could imagine that the daily reality they were now living could be anything other than the end of the world. And this mindset and the psychology that undergirded it led to massive changes in society and human thought that may be without rival in human history.
References
Chapter 15 Cover Photo: Black death. Public Domain (from Toggenburg Bible). Accessed via commons.wikimedia.org
Figure 15.1: Flea. CC0 Public Domain: WikiImages. Accessed via https://pixabay.com/en/flea-siphonaptera-insect-parasite-63043/
Figure 15.2: Grasshopper digestive system. Author unknown. Accessed via http://www.earthlife.net/insects/anat-abdomen.html
Figure 15.3: Flea digestive system. From Hinnebusch, B.J. (2005). The evolution of flea-borne transmission in Yersinia pestis. Curr Issues Mol Biol. Jul 7(2): 197-212. Available at https://www.ncbi.nlm.nih.gov/pubmed/16053250
Figure 15.4: Human plague in the U.S.. Centers for Disease Control and Prevention. Accessed via https://www.cdc.gov/plague/maps/
Figure 15.5: Transmission cycle of The Black Death. S. W. Fisher, own work.
Figure 15.6: The Black Death from the Toggenburg Bible. CC0 Public Domain. Accessed via https://commons.wikimedia.org/wiki/File:Smallpox_depicted_in_the_Toggenburg_Bible.jpg
Table 15.1: Forms of plague. Information compiled by S. W. Fisher
Additional Readings
Aleksic, S. and Bockemuhl, J.(1999). Yersinia and other Enterobacteriaceae. In: Manual of Clinical Microbiology, 7th ed.
Alibek, K. and S. Handelman (1999). Biohazard. Random House, New York, NY.
Boyce, J.M. and Butler, T., 1995. Yersinia species (including plague). Principles and Practice of Infectious Diseases, 4th ed. New York: Churchill Livingstone, pp.2070-2078.
Centers for Disease Control and Prevention, Maps and Statistics. Plague in the United StatesSep 14, 2015 www.cdc.gov/plague/maps/
Derbes, V.J. (1996). De Mussis and the Great Plague of 1348: A Forgotten Episode of Bacteriological War. JAMA 196: 59-62.
Harris, S. H. (1994). Factories of Death. Routledge, New York, NY.
Hinnebusch, B.J. (2005). The Evolution of Flea-borne Transmission in Yersinia pestis. Current Issues Molecular Biology 7: 197-212.
Inglesby, T.V., D.T. Dennis, D.A. Henderson, J.G. Bartlett, M.S. Ascher, E.Eitzen, A.D. Fine, A. M. Friedlander, J. Hauer, J.F. Koerner, M. Layton, J. McDade, M.T. Osterholm, T. O’Toole, G. Parker, T. M. Perl, P. K. Russell, M. Schoch-Spana, and K. Tonat (2000). Plague as a Biological Weapon: Medical and Public Health Management. JAMA 283: 2281-2290.
Perry, R.D. and J.D. Fetherson (1997). Yersinia pestis—Etiologic Agent of Plague. Clin. Microbiol. Rev. 10: 35-66.
Schmid, B.V., U.Buntgen, W.R. Easterday, C.Ginzler, L. Walloe, B. Brammanti and N. C. Stenseth (2014). Climate-driven Introduction of the Black Death and Successive Plague Reintroductions into Europe. Proc. Nat. Acad. Sci.org.cgi.doi/10.1073/pnas.1412887112.
Slack, P. (1989). The Black Death Past and Present. Trans. R. Soci Trop. Med. Hyg. 83: 461-463.
Zhou, D., Y. Han and R. Yang (2005). Molecular and physiological insights into plague transmission, virulence and etiology. Doi:10.1016/j.micinf.2005.06.006.
Wheelis, M. (2002). Biological Warfare at the 1346 Siege of Caffa. Emerging Infectious Diseases 8: 971-975.