Ch. 2: A Brief History of Substance Use and Policy Responses in the U.S.
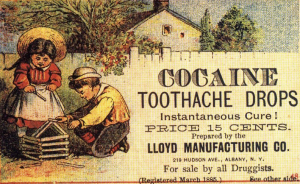 While substance misuse is a contemporary social problem, the story of humans experiencing problems related to the use of psychoactive substances is at least 4,000-10,000 years old (Hanson, Venturelli, & Fleckenstein, 2015; Howard, Garland, & Whitt, 2013; Singer, 2012). United States history is peppered with documentation of problems associated with alcohol and other drugs. For example, the opiate drug morphine was widely used during the Civil War to manage wounded soldiers’ pain, leaving many of them experiencing morphine addiction as a result. Subsequently, heroin became available and marketed as a “non-addicting opiate with greater analgesic potency than morphine” (Kornetsky, 2007, p. 96). Prior to the Civil War, 60-75% of Americans experiencing opium or morphine addiction were women, in large part because physicians often prescribed opiates to deal with a wide variety of “female” complaints (Blumenthal, 1998). In addition, physicians of the time often prescribed alcohol as a treatment for opiate addiction, and many socially acceptable and widely accessible medicines contained very high alcohol or opium content (Plant, 1997; Straussner & Attia, 2002; van Wormer & Davis, 2013). Cocaine was also prescribed and marketed in this way. See this historic advertisement promising an instant cure for oral pain (including babies’ teething pain).
While substance misuse is a contemporary social problem, the story of humans experiencing problems related to the use of psychoactive substances is at least 4,000-10,000 years old (Hanson, Venturelli, & Fleckenstein, 2015; Howard, Garland, & Whitt, 2013; Singer, 2012). United States history is peppered with documentation of problems associated with alcohol and other drugs. For example, the opiate drug morphine was widely used during the Civil War to manage wounded soldiers’ pain, leaving many of them experiencing morphine addiction as a result. Subsequently, heroin became available and marketed as a “non-addicting opiate with greater analgesic potency than morphine” (Kornetsky, 2007, p. 96). Prior to the Civil War, 60-75% of Americans experiencing opium or morphine addiction were women, in large part because physicians often prescribed opiates to deal with a wide variety of “female” complaints (Blumenthal, 1998). In addition, physicians of the time often prescribed alcohol as a treatment for opiate addiction, and many socially acceptable and widely accessible medicines contained very high alcohol or opium content (Plant, 1997; Straussner & Attia, 2002; van Wormer & Davis, 2013). Cocaine was also prescribed and marketed in this way. See this historic advertisement promising an instant cure for oral pain (including babies’ teething pain).
At around the end of the 19th century, awareness of potential harms associated with these substances spread. The U.S. (and other nations) has since implemented various policy efforts to reduce both or either supply and demand for different kinds of drugs (Vakharia & Little,in press). Protecting public health was not the only motivation in many instances, however.
Early U.S. Policy and Legislation Efforts.
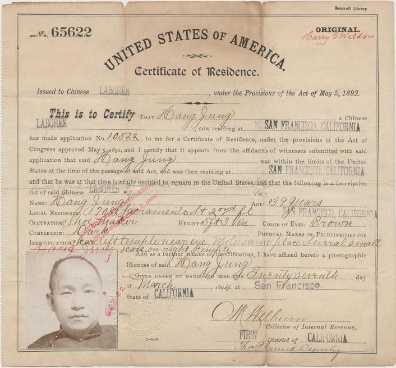 The first federal policy prohibiting distribution (supply) and non-medical use (demand) of a drug was the Opium Exclusion Act of 1909 (Vakharia & Little, in press). Opium used for medical purposes remained legal, but opium prepared for “smoking” no longer was. At this point in history, large numbers of Chinese immigrants were working in the U.S. and opium smoking was associated with this population. The common use was not outlawed, only the form of opium used by Chinese immigrants (Vakharia & Little, in press).
The first federal policy prohibiting distribution (supply) and non-medical use (demand) of a drug was the Opium Exclusion Act of 1909 (Vakharia & Little, in press). Opium used for medical purposes remained legal, but opium prepared for “smoking” no longer was. At this point in history, large numbers of Chinese immigrants were working in the U.S. and opium smoking was associated with this population. The common use was not outlawed, only the form of opium used by Chinese immigrants (Vakharia & Little, in press).
The next major federal policy, the Harrison Narcotic Act of 1914, was directed at drugs derived from opium or coca leaves, to control their production, distribution, and use. Possession or use of a narcotic (this included cocaine) without a physician’s prescription was a violation that states could criminalize. Cocaine was targeted, possibly for political reasons parallel to the situation with opium (Vakharia & Little, in press): up until the early 1900s, cocaine was commonly added to beverages and medicinal tonics because of its energizing properties (and boosting worker productivity). Even though most individuals using cocaine were white, concern grew over its increasing popularity within the black community, particularly across the Southern U.S. (Vakharia & Little, in press). An added public policy motivation: governments could now collect special taxes on the production and distribution of these drugs. Tobacco has been taxed at the federal and state levels since the Civil War, with the amount fluctuating (until 1983) according to governments’ need to generate revenue (IOM,1994).
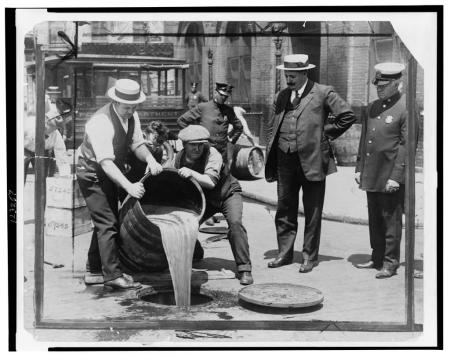
The Harrison Narcotic Act represented early prohibition efforts and laid the foundation for much of the substance-related policy enacted in the U.S. and by individual states or local communities, including marijuana and alcohol control efforts (Vakharia & Little, in press). In attempting to prevent the spread of alcohol or other drug addiction, some public policies advocated institutionalization in psychiatric or criminal facilities, as well as forced sterilization as part of the negative eugenics movement (Straussner & Attia, 2002; White, 1998). One effort with which you may be somewhat familiar was passage of the 18th Amendment—commonly known as Prohibition. The 18th Amendment to the United States Constitution banned the manufacture, sale, or transportation of “intoxicating liquors,” but not the drinking of alcoholic beverages. (This picture shows agents pouring liquor confiscated in a New York City raid during Prohibition; it comes from the National Archives).
Prohibition Era.
 Although the combination of the 18thAmendment to the United States Constitution and the Volstead Act (which clarified that beer and wine were included as alcoholic beverages) were implemented beginning in 1920, many states had already enacted their own local prohibition laws (Hanson, Venturelli, & Fleckenstein, 2015; Kelly, 2017). You might find it interesting to pursue historical literature documenting the intersections of alcohol/drug policy with historical and sociological trends such as the temperance movement, women’s suffrage, immigration, organized crime, classism and racism (see for example, Straussner & Attia, 2002; van Wormer & Davis, 2013). Many of these historical policy patterns have implications for today’s politics and policy debates, as does the extensive economic impact of both local and international trade in substances such as alcohol, tobacco, coffee, tea, opium, cocaine, and others.
Although the combination of the 18thAmendment to the United States Constitution and the Volstead Act (which clarified that beer and wine were included as alcoholic beverages) were implemented beginning in 1920, many states had already enacted their own local prohibition laws (Hanson, Venturelli, & Fleckenstein, 2015; Kelly, 2017). You might find it interesting to pursue historical literature documenting the intersections of alcohol/drug policy with historical and sociological trends such as the temperance movement, women’s suffrage, immigration, organized crime, classism and racism (see for example, Straussner & Attia, 2002; van Wormer & Davis, 2013). Many of these historical policy patterns have implications for today’s politics and policy debates, as does the extensive economic impact of both local and international trade in substances such as alcohol, tobacco, coffee, tea, opium, cocaine, and others.
The 21stAmendment repealed the federal alcohol prohibition laws in late 1933; some states and local jurisdictions were slower to change their own prohibition policies. Some states continue to have “dry” communities restricting the sale or distribution of alcohol, and some communities maintain “Sunday” or “blue” laws banning the sale of alcohol during certain hours.
 It was also during the 1920s and 1930s that many states developed prohibition-style policies about marijuana, and the federal government got involved in 1937 with the passage of a Marijuana Tax Act and more severe criminalization policies during the 1950s. Marijuana policy concerns cannabis plant products; the word marijuana came from Mexico, but its use in U.S. policy is becoming recognized as having racist and propagandist connotations by many scholars (Malcolm, in press). Historical roots of marijuana prohibition include racial/ethnic concerns about Mexican immigrants and African Americans that parallel opium and cocaine policy regarding Chinese immigrants and Southern black workers (Malcolm, in press).
It was also during the 1920s and 1930s that many states developed prohibition-style policies about marijuana, and the federal government got involved in 1937 with the passage of a Marijuana Tax Act and more severe criminalization policies during the 1950s. Marijuana policy concerns cannabis plant products; the word marijuana came from Mexico, but its use in U.S. policy is becoming recognized as having racist and propagandist connotations by many scholars (Malcolm, in press). Historical roots of marijuana prohibition include racial/ethnic concerns about Mexican immigrants and African Americans that parallel opium and cocaine policy regarding Chinese immigrants and Southern black workers (Malcolm, in press).
Evolution of Contemporary U.S. Drug Policy.
 During the 1960s, many programs and policies aimed at addressing both the supply and the demand sides of the drug trade were established. The term “War on Drugs” began to appear around 1971, referring to stepped-up drug criminalization and law enforcement efforts (McNeece & DiNitto, 2012; Schori & Lawental, 2013). While these programs focused on our nation’s internal drug problem, it is virtually impossible to separate the U.S. drug war efforts from international policy, international relations, and global economics. It also had political undertones and overtones related to race, age, and the “counter-culture” presence in America at the time.
During the 1960s, many programs and policies aimed at addressing both the supply and the demand sides of the drug trade were established. The term “War on Drugs” began to appear around 1971, referring to stepped-up drug criminalization and law enforcement efforts (McNeece & DiNitto, 2012; Schori & Lawental, 2013). While these programs focused on our nation’s internal drug problem, it is virtually impossible to separate the U.S. drug war efforts from international policy, international relations, and global economics. It also had political undertones and overtones related to race, age, and the “counter-culture” presence in America at the time.
One criticism of “America’s Longest War” (the title of a 2013 award-winning documentary) has great relevance to social work and disciplines concerned with social justice: the War on Drugs contributed to extreme racial and gender inequities in the nation’s incarceration rates (Bush-Baskette, 1999; Chesney-Lind, 1997). For example, by the early 1990s, 74% of individuals serving prison sentences for drug possession were black, despite accounting for only 13% of individuals who use drugs (Kilty & Joseph, 1999). The War on Drugs also helps explain the relative explosion of women in prison for non-violent, drug possession charges that occurred during the late 1980s to 1990s—leading to a declaration that the War on Drugs became a “War on Women” (Bloom, Chesney Lind, & Owen, 1994). Another criticism of the War on Drugs addresses its high economic costs: the Office of National Drug Control Policy’s (ONDCP) FY 2020 National Drug Control Budget request was $34.6 billion, an increase of $1.3 billion over the actual FY 2019 budget (https://www.whitehouse.gov/briefings-statements/white-house-seeks-billions-record-investments-stop-drug-epidemic/). The ONDCP is a component of the President’s White House Executive Office, created by the 1988 Anti-Drug Abuse Act.
Pregnant Women and Substance Use.
 Part of the concern about a “War on Women” stems from how policy responses (mostly at the state level) to women’s use of alcohol or other drugs (AOD) during pregnancy. States and local communities differ markedly in their policy responses to this issue. The responses run the gamut from dealing with the public health aspects (the health of mother and baby) to criminalization. For example, in some states, a pregnant woman can be involuntarily committed to a treatment facility, jail, or relative’s home for supervision to prevent her continued use of substances known to be harmful to a developing fetus. Many states have policies relating to the substantiation of child maltreatment allegations when a pregnant mother uses alcohol or other drugs. While intended to help protect the unborn child from potentially harmful drug exposure, these policies are controversial, as they also may discourage women from seeking much-needed prenatal care for fear of discovery and becoming subject to consequences imposed through the courts and child welfare system.
Part of the concern about a “War on Women” stems from how policy responses (mostly at the state level) to women’s use of alcohol or other drugs (AOD) during pregnancy. States and local communities differ markedly in their policy responses to this issue. The responses run the gamut from dealing with the public health aspects (the health of mother and baby) to criminalization. For example, in some states, a pregnant woman can be involuntarily committed to a treatment facility, jail, or relative’s home for supervision to prevent her continued use of substances known to be harmful to a developing fetus. Many states have policies relating to the substantiation of child maltreatment allegations when a pregnant mother uses alcohol or other drugs. While intended to help protect the unborn child from potentially harmful drug exposure, these policies are controversial, as they also may discourage women from seeking much-needed prenatal care for fear of discovery and becoming subject to consequences imposed through the courts and child welfare system.
Drinking Age Legislation.
 Drinking age legislation in the U.S. currently aims to restrict alcohol use by persons under the age of 21 years. You may find it hypocritical that an 18-year-old person is treated as an adult in other domains (legal rights to marry, join the military, enter into legal contracts), but not legally allowed to purchase alcohol. Drinking establishments are certainly concerned about reduced revenue from not being allowed to legally serve alcohol to 18- to 20-year-olds. On the other hand, there exists compelling evidence that higher drinking age minimums are associated with lower traffic fatality rates. Another rationale involves an attempt to mitigate the potential harms associated with exposing the still-developing young adult brain to alcohol—major developmental changes in brain structure and function, beginning early in puberty, continue well into the period of early adulthood (Spear, 2000; more about this in our focus on alcohol module). Raising the legal age to be well over 18 eliminates confusion about enforcing alcohol-free zones in high schools and many parts of college/university life, as well. This policy periodically becomes contested, tested, and retested in the United States, including a period during the 1970s when different states had different legal drinking ages of 18, 19, and 21. Drinking age policy is determined at the state level, however federal highway funding is tied to state drinking age policy and governing the states’ uniform decision to support a minimum legal drinking age of 21 years.
Drinking age legislation in the U.S. currently aims to restrict alcohol use by persons under the age of 21 years. You may find it hypocritical that an 18-year-old person is treated as an adult in other domains (legal rights to marry, join the military, enter into legal contracts), but not legally allowed to purchase alcohol. Drinking establishments are certainly concerned about reduced revenue from not being allowed to legally serve alcohol to 18- to 20-year-olds. On the other hand, there exists compelling evidence that higher drinking age minimums are associated with lower traffic fatality rates. Another rationale involves an attempt to mitigate the potential harms associated with exposing the still-developing young adult brain to alcohol—major developmental changes in brain structure and function, beginning early in puberty, continue well into the period of early adulthood (Spear, 2000; more about this in our focus on alcohol module). Raising the legal age to be well over 18 eliminates confusion about enforcing alcohol-free zones in high schools and many parts of college/university life, as well. This policy periodically becomes contested, tested, and retested in the United States, including a period during the 1970s when different states had different legal drinking ages of 18, 19, and 21. Drinking age policy is determined at the state level, however federal highway funding is tied to state drinking age policy and governing the states’ uniform decision to support a minimum legal drinking age of 21 years.
Decriminalization Efforts.
 Our nation has an opportunity to learn from the contemporary “natural experiment” in policy reform whereby several states decriminalized the production, distribution, possession, and/or use of cannabis for medical and/or recreational purposes (more about this in our focus on cannabis module). Some hypothesize that decriminalization of substance possession or use reduces economic incentives for illegal production and distribution of drugs, allowing government entities to increase revenue through taxation (McNeece & DiNitto, 2012). Decriminalization is contested, however, as potentially contributing to increased rates of substance use disorders and other health risks associated with substance use, as well as related problems such as driving under the influence and community safety. Law enforcement professionals expressed grave concerns regarding the potential for increased demands on police forces already stretched by the need to manage alcohol-related situations if marijuana is also legally used by the general public. Recent evidence suggests that the presence of legal (medical) marijuana dispensaries are associated with increased violent and property crime rates in adjacent areas (Freisthler, Ponicki, Gaidus, & Gruenwald, 2016).
Our nation has an opportunity to learn from the contemporary “natural experiment” in policy reform whereby several states decriminalized the production, distribution, possession, and/or use of cannabis for medical and/or recreational purposes (more about this in our focus on cannabis module). Some hypothesize that decriminalization of substance possession or use reduces economic incentives for illegal production and distribution of drugs, allowing government entities to increase revenue through taxation (McNeece & DiNitto, 2012). Decriminalization is contested, however, as potentially contributing to increased rates of substance use disorders and other health risks associated with substance use, as well as related problems such as driving under the influence and community safety. Law enforcement professionals expressed grave concerns regarding the potential for increased demands on police forces already stretched by the need to manage alcohol-related situations if marijuana is also legally used by the general public. Recent evidence suggests that the presence of legal (medical) marijuana dispensaries are associated with increased violent and property crime rates in adjacent areas (Freisthler, Ponicki, Gaidus, & Gruenwald, 2016).
Addiction treatment providers have expressed concern about the potential impact of easier access on individuals already in recovery from substance use disorders and the potential for further stressing an under-resourced service delivery system with an increase in demand for intervention to address problems with marijuana use. Prevention experts are concerned about the message that legalization/decriminalization might convey to young people considering initiating substance use. And, there continues to be controversy as to the potential (as yet, unknown) effects on the health care system that might result from an increase in disease or disability resulting from individuals’ long-term use of marijuana products—along the lines of what we see with alcohol.

However, social justice advocate relates significant inequities in how the criminalization of cannabis and other drugs is enforced, leading to both a mass incarceration trend and tremendous racial/ethnic (and gender) disparities in who becomes incarcerated in the nation’s, states’, and local communities’ jails and prisons. Mass incarceration beginning in the mid-1970s meant the incarceration rate almost tripled from 1970 (96 per 100,000 population) to 1990 (over 300 per 100,000; Lloyd & Fendrich, in press). Not only were War on Drugs policies responsible for this trend, so were policies and policy enforcement stemming from Sentencing Reform Act (1984), Anti-Drug Abuse Act (1986), and Omnibus Anti-Drug Abuse Act (1988) policies concerning sentencing guidelines establishing mandatory minimum penalties for drug crimes (Lloyd & Fendrich,in press). Disparities in incarceration of persons of color were further stimulated by differential sentencing for “crack” cocaine (more commonly used by persons of color) compared to powdered cocaine (used by more affluent and white individuals). Advocating for “smart decarceration” often means advocating for less punitive (and more treatment) responses for low-level and non-violent drug involvement (see Pettus-Davis & Epperson, 2015).
Drug courts.
 Traditional drug-control methods of the criminal justice system, such as mandatory incarceration and harsher penalties, along with court-mandated treatment following release from incarceration, have not proven to be sufficiently effective to curb the problems associated with illicit drug use (Broadus, 2009). In addition, these efforts were wreaking havoc on the court system by creating tremendous backlogs of cases considered to involve relatively minor, non-violent offenses, and pushing jail populations far over capacity at great public expense. In response, a movement emerged during the early-1990s to establish special courts for managing nonviolent drug-related cases. The mission was to engage individuals in court-monitored, structured, evidence-supported treatment and divert them from being incarcerated if they complied with the treatment plan. By 2018, over half of all U.S. counties sponsored at least one of over 3,100 drug courts in operation (Lloyd & Fendrich, in press). Each program involves an interdisciplinary team of criminal justice and mental health professionals responsible for creating an individualized comprehensive plan for each program participant and monitoring participant progress. Failure to comply with the court-treatment plan results in the court levying the traditional sentences for the original offenses. Short-term outcome studies support the drug court model as participants, on average, remain in treatment longer than in traditional treatment settings and experience fewer relapse events, recidivism rates are lower, and participants are able to improve education, housing, and health, as well. Results generally are not as promising for juvenile drug courts as for adult drug court (Lloyd & Fendrich, in press).
Traditional drug-control methods of the criminal justice system, such as mandatory incarceration and harsher penalties, along with court-mandated treatment following release from incarceration, have not proven to be sufficiently effective to curb the problems associated with illicit drug use (Broadus, 2009). In addition, these efforts were wreaking havoc on the court system by creating tremendous backlogs of cases considered to involve relatively minor, non-violent offenses, and pushing jail populations far over capacity at great public expense. In response, a movement emerged during the early-1990s to establish special courts for managing nonviolent drug-related cases. The mission was to engage individuals in court-monitored, structured, evidence-supported treatment and divert them from being incarcerated if they complied with the treatment plan. By 2018, over half of all U.S. counties sponsored at least one of over 3,100 drug courts in operation (Lloyd & Fendrich, in press). Each program involves an interdisciplinary team of criminal justice and mental health professionals responsible for creating an individualized comprehensive plan for each program participant and monitoring participant progress. Failure to comply with the court-treatment plan results in the court levying the traditional sentences for the original offenses. Short-term outcome studies support the drug court model as participants, on average, remain in treatment longer than in traditional treatment settings and experience fewer relapse events, recidivism rates are lower, and participants are able to improve education, housing, and health, as well. Results generally are not as promising for juvenile drug courts as for adult drug court (Lloyd & Fendrich, in press).
Harm Reduction Policies.
Some strategies and policy approaches are based on a principle that has come to be known as harm reduction. While the goal always remains reducing substance misuse risk by ending high-risk substance use behaviors (alcohol or other drugs), it is not always wisest to wait for risky behaviors to cease. While waiting, harms to individuals, families, and communities accumulate. Instead, often it is wiser to intervene in ways that reduce the potential risks, harms, and other negative consequences associated with the behaviors in the meantime. The harm reduction approach, derived from public health rather than criminalization motivations, aims to improve quality of life for individuals, families, and communities associated with the risky behaviors (Collins et al., 2012). Some harm reduction policy examples include:
- programs to prevent driving while under the influence of alcohol or other substances, while not necessarily stopping a person from using AOD;
- clean needle and syringe exchange programs to reduce risk of exposure to blood-borne communicable diseases like HIV/AIDS and hepatitis;
- supervised drug-use settings where individuals’ drug use and safety are monitored by someone whose judgement is not substance-impaired (more common in European nations);
- fentanyl testing of heroin/opioids or other “street” drugs to prevent unexpected opioid overdose;
- supportive housing for which abstinence is not an eligibility requirement;
- making opioid overdose reversal resources (Narcan) available to first responders to save the lives of individuals who might otherwise die before professional treatment is accessible.
On one hand, harm reduction is viewed as being practical and humane. Harm reduction programs may also serve as pathways to enter treatment and reduce substance misuse. On the other hand, some argue that harm reduction is too “soft” on individuals who break the law through substance misuse abstinence-only policies are necessary to stop the harms caused by substance misuse, and risk-reduction approaches do not do enough to stop substance misuse. In addition to harm reduction policies, there exist treatment intervention approaches in the harm reduction spirit, as well.
Access to Treatment.
 Improving access to treatment for substance misuse and substance use disorders represents another modern policy/advocacy front with great social work significance. In the previous epidemiology sections, you learned about the considerable gap that exists between the need for these services and the numbers of individuals (and families) able to receive them. A person’s ability to engage in formal, professional treatment for these problems often depends on the ability to pay with insurance or self-pay dollars.
Improving access to treatment for substance misuse and substance use disorders represents another modern policy/advocacy front with great social work significance. In the previous epidemiology sections, you learned about the considerable gap that exists between the need for these services and the numbers of individuals (and families) able to receive them. A person’s ability to engage in formal, professional treatment for these problems often depends on the ability to pay with insurance or self-pay dollars.
One potential advantage of the Affordable Care Act (ACA) first implemented in the United States during 2013-2014 was the potential for increased access to mental health and substance use disorder treatment services for many individuals. With the passage of the ACA:
- young people could remain on a parent’s Medicaid plan until the age of 26 years (remember that 18-25 was the age period the greatest number of individuals engaged in substance misuse);
- subsidies helped more individuals afford health insurance;
- annual and lifetime benefit limits and limits on the number of visits for behavioral health services were eliminated;
- behavioral health care became more affordable by ensuring co-pay expenses could not be greater than those for physical health services; and,
- insurability was protected for individuals experiencing a pre-existing condition in their medical records (having a history of a substance use disorder would be a pre-existing condition necessitating protections, no matter how long the person has been in recovery).
The federal Mental Health Parity and Addiction Equity Act of 2008 also helped regulate the health plan/insurance industry regarding benefits for individuals with substance use disorders in their medical histories.
Despite the excitement over expanded coverage and protections, concerns arose regarding the treatment system’s ability to meet the anticipated increase in demand: Do we have enough trained professionals to meet the experienced need?
 At the end of 2016, the U.S. Congress passed two major pieces of legislation related to substance use and addiction. The first was the Comprehensive Addiction and Recovery Act (CARA) that provided legal status for many harm reduction strategies, such as increased access by non-physicians to naloxone for reversing an opioid overdose. However, CARA did not provide funding for these approaches. The second was the 21stCentury Cures Act that provided federal funding to “accelerate the discovery, development, and delivery of 21stcentury cures” and other purposes (https://www.congress.gov/bill/114th-congress/house-bill/34/text). In addition to ensuring specific funding for the NIH and Federal Drug Administration, the act provided funding for states with a relatively high prevalence of opioid use disorders to develop their responses for addressing the opioid abuse crisis. This included prescription drug monitoring programs, prevention activities, health care provider training about best practices, supporting access to treatment programs, and other public health-related activities to address the identified crisis. The impact of policy revisions regarding health care coverage since the 2017 change in national leadership remains to be seen. The White House created the President’s Commission on Combatting Drug Addiction and the Opioid Crisis (March 2017) with the mission of studying “the scope and effectiveness of the Federal response to drug addiction and the opioid crisis…and make recommendations to the President for improving that response” (https://www.whitehouse.gov/the-press-office/2017/03/30/presidential-executive-order-establishing-presidents-commission). However, at the same time, the Office of National Drug Control Policy, a component of the President’s Executive Office, risked being significantly defunded. Clearly, there exists considerable ambivalence in the policy response to substance misuse and treatment for substance use disorders in the U.S.
At the end of 2016, the U.S. Congress passed two major pieces of legislation related to substance use and addiction. The first was the Comprehensive Addiction and Recovery Act (CARA) that provided legal status for many harm reduction strategies, such as increased access by non-physicians to naloxone for reversing an opioid overdose. However, CARA did not provide funding for these approaches. The second was the 21stCentury Cures Act that provided federal funding to “accelerate the discovery, development, and delivery of 21stcentury cures” and other purposes (https://www.congress.gov/bill/114th-congress/house-bill/34/text). In addition to ensuring specific funding for the NIH and Federal Drug Administration, the act provided funding for states with a relatively high prevalence of opioid use disorders to develop their responses for addressing the opioid abuse crisis. This included prescription drug monitoring programs, prevention activities, health care provider training about best practices, supporting access to treatment programs, and other public health-related activities to address the identified crisis. The impact of policy revisions regarding health care coverage since the 2017 change in national leadership remains to be seen. The White House created the President’s Commission on Combatting Drug Addiction and the Opioid Crisis (March 2017) with the mission of studying “the scope and effectiveness of the Federal response to drug addiction and the opioid crisis…and make recommendations to the President for improving that response” (https://www.whitehouse.gov/the-press-office/2017/03/30/presidential-executive-order-establishing-presidents-commission). However, at the same time, the Office of National Drug Control Policy, a component of the President’s Executive Office, risked being significantly defunded. Clearly, there exists considerable ambivalence in the policy response to substance misuse and treatment for substance use disorders in the U.S.

Before you read on, take a moment to jot down your “best guess” answers to the following questions:
Thinking About Policy Issues
For each of the following topics, consider what evidence supports your position, and what evidence might counter your position.
- Drinking Age Legislation: What do you think about the current minimum legal drinking age policies in the United States? What do you know about policies in your own community regarding being a minor in possession of alcohol, driving while under the influence as a minor, and the provision of alcohol to underage minors? How might these issues apply to cigarettes, e-cigarettes, and other tobacco products?
- Drinking or Drug Use during Pregnancy: What do you think should be the state’s policy and why? What are the social justice issues involved? What are the likely “real world” implications of implementing (or not) such ideas in practice.
- Prohibiting versus Decriminalizing Policies: Thinking about the historical policy called Prohibition, what are the parallels and differences with regard to policies restricting distribution and use of other substances like marijuana, opioids and heroin. Consider the effectiveness or ineffectiveness of public education strategies that involve “scare tactics” and “Just Say No” policy responses to preventing substance use initiation by young people–what worked and what did not, and for whom were these approaches effective and for whom were they problematic? Why do you think the problems were or were not solved this way?
- Naloxone access: Naloxone is not a cure for addiction, but the immediate life-or-death health crisis may be resolved if delivered in time. There is no question that many lives have been saved (in the short-term, at least) with this overdose reversal intervention. The wholesale price for a 3-dose administration (more than one dose is often necessary for individuals who used heroin/fentanyl combinations) can cost over $4,200. Though the costs to an individual person or family member can be offset to between $0-$125 in some communities through donated doses, grants, and public funding, the cost of doses provided by first responders may or may not be offset.
- What do you think about policy allowing laypersons in the community to obtain naloxone to use if they witness an opioid overdose (e.g., a friend, family member, or someone else using drugs together)?
- What about providing it individuals with diagnosed opioid addiction, to carry for others to administer if they overdose?
- How do you feel about doing this for someone yourself (and perhaps conduct rescue breathing during the time it takes to work)?
- How do you feel about these costs affecting city/county/state budgets for first responders?
- How do you feel about pharmaceutical companies charging so much for this life-saving treatment, despite their having invested heavily in its development and testing?
