Ch. 2: Family as Social Context
There is no doubt that substance misuse and substance disorders often seem to “run” in families. We explored genetic models in Module 3 and learned that expression of genetic vulnerability or resilience to addiction is heavily influenced by environment and experience. The family system is a powerful source of environmental influence to consider. This chapter explores the family as one influential social context of substance use initiation, substance misuse, substance use disorder, and recovery.
Family forms a context for a great deal of human development—it is a site where individuals learn behaviors through operant conditioning (reinforcement and punishment of their behaviors) and observational learning (behavioral models), as well as become socialized into their culture, social norms, and social roles. The physical environment established by a family can also influence development and behavior through constraints and opportunities provided to individuals—for example, ease of access to alcohol, tobacco products, or other psychoactive substances. Family social relationships influence a person’s motivation for social conformity or deviance, as well. Family can be a source of stress to which a person might respond with substance use, or a source of resilience and protective factors that reduce the probability of engaging in substance misuse.
Family Systems Theory
Not only do we need to consider how learning, social learning, social norms, and cultural beliefs related to alcohol and other substances operate within families, we also need to consider how family system principles apply to the situation. A prevailing principle in family systems theory concerns families’ conscious or subconscious efforts to establish and maintain a stable state of homeostasis or balance. Just like a biological organism (e.g., the human body), family systems tend to develop practices, roles, rules, norms, patterns of communication and behaviors that serve this homeostatic function. Consider, for example, a family “rule” about not discussing or tending to minimize a member’s substance misuse. Making the topic taboo might be dysfunctional in terms of getting the substance misuse problem addressed but may serve the family’s need to maintain a stable peace despite the problem. Here is a brief orientation to four facets of the family systems theory as applied to individual members’ substance misuse (see Begun, Hodge, & Early, 2017).
- The family is a system embedded in other, larger social systems. Just as we saw the individual embedded in micro- to macro-level systems in the social ecological framework, family systems also are embedded in progressively larger social systems. We cannot hope to understand families or their behavior, functioning, and development without understanding their interactions with their ecological contexts—the influences of extended family, neighborhood, social institutions, culture, society, and large-scale political, economic, and historical trends. Consider, for example, the influence of local, national, and global economy on families in your own community.

 In this framework, consider how family contexts might influence individuals’ substance use behavior, treatment seeking, and recovery-related behaviors and the ways that family supports or challenges their substance use behavior or recovery efforts. For example, how might a family’s relationships with religious/spiritual systems, education or workplace settings, neighborhood, criminal justice system, child welfare system, and others be relevant in preventing substance use initiation or substance use from becoming misuse or a substance use disorder? Individuals are not only a product of (and influence on) interactions with the nuclear family but also of the family’s interactions with extended family—how might extended kin relationships impact the behaviors of an individual family member? Or, for example, how do kin play a role in caring for children when a parent is engaging in substance misuse or working on recovery (as discussed in a chapter about grandfamilies by Mendoza, Fruhauf, and Hayslip, in press). A number of interventions for individuals experiencing substance use disorder are designed to involve families and supportive significant others (SSOs) in the process, as well as provide support to these families/SSOs in their own right (e.g., as discussed in chapters about working with children and families of individuals engaged in substance misuse by Straussner and Fewell, in press, and by Petra and Kourgiantakis, in press). Considering the neighborhood, organization, and community levels, crime and violence in a neighborhood might be relevant because it affects family stress and distress levels, which in turn may influence substance use at the individual level; access to preventive and treatment interventions in the community are also relevant features of the family’s context.
In this framework, consider how family contexts might influence individuals’ substance use behavior, treatment seeking, and recovery-related behaviors and the ways that family supports or challenges their substance use behavior or recovery efforts. For example, how might a family’s relationships with religious/spiritual systems, education or workplace settings, neighborhood, criminal justice system, child welfare system, and others be relevant in preventing substance use initiation or substance use from becoming misuse or a substance use disorder? Individuals are not only a product of (and influence on) interactions with the nuclear family but also of the family’s interactions with extended family—how might extended kin relationships impact the behaviors of an individual family member? Or, for example, how do kin play a role in caring for children when a parent is engaging in substance misuse or working on recovery (as discussed in a chapter about grandfamilies by Mendoza, Fruhauf, and Hayslip, in press). A number of interventions for individuals experiencing substance use disorder are designed to involve families and supportive significant others (SSOs) in the process, as well as provide support to these families/SSOs in their own right (e.g., as discussed in chapters about working with children and families of individuals engaged in substance misuse by Straussner and Fewell, in press, and by Petra and Kourgiantakis, in press). Considering the neighborhood, organization, and community levels, crime and violence in a neighborhood might be relevant because it affects family stress and distress levels, which in turn may influence substance use at the individual level; access to preventive and treatment interventions in the community are also relevant features of the family’s context.
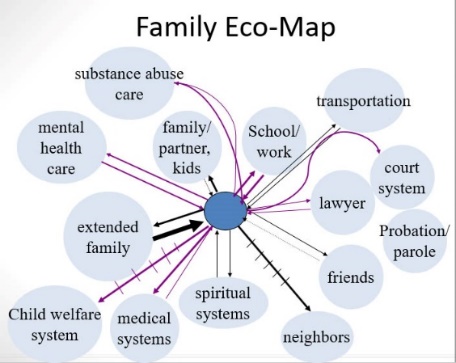 An eco-map is a visual assessment tool (originally described by Dr. Ann Hartmann) used in social work to help families identify and express the nature and quality of their interactions with the surrounding systems—what is supportive and what is detrimental, where the energy, emotional, and resource “costs” to the family are excessive compared to what is gained, and where the “gains” are more favorable than the costs. In some cases, a family eco-map may appear overly sparse, leaving the family under-resourced and socially isolated. At the other extreme, a family’s eco-map may be overly saturated with formal institutions that serve the family but at a high “cost” in effort and energy; even informal relationships are supported at some cost since they typically exist within a set of “give and take” expectations. Even if the amount and types of ecological relationships may be reasonably balanced, the qualitative picture may be heavily conflict-ridden as opposed to working peacefully or harmoniously. For example, when a family member engages in substance misuse involvement with criminal justice, child welfare, housing, and health care systems may occur, much of which is demanding despite possibly providing needed resources. All of this relates to the degree of stress which the family system is under in its day-to-day existence. Stress is often translated into individuals’ use of substances, according to stress and coping theory which emphasizes the stress experienced in contexts characterized by a great deal of social disorganization, distress, and alienation (Moos, 2006).
An eco-map is a visual assessment tool (originally described by Dr. Ann Hartmann) used in social work to help families identify and express the nature and quality of their interactions with the surrounding systems—what is supportive and what is detrimental, where the energy, emotional, and resource “costs” to the family are excessive compared to what is gained, and where the “gains” are more favorable than the costs. In some cases, a family eco-map may appear overly sparse, leaving the family under-resourced and socially isolated. At the other extreme, a family’s eco-map may be overly saturated with formal institutions that serve the family but at a high “cost” in effort and energy; even informal relationships are supported at some cost since they typically exist within a set of “give and take” expectations. Even if the amount and types of ecological relationships may be reasonably balanced, the qualitative picture may be heavily conflict-ridden as opposed to working peacefully or harmoniously. For example, when a family member engages in substance misuse involvement with criminal justice, child welfare, housing, and health care systems may occur, much of which is demanding despite possibly providing needed resources. All of this relates to the degree of stress which the family system is under in its day-to-day existence. Stress is often translated into individuals’ use of substances, according to stress and coping theory which emphasizes the stress experienced in contexts characterized by a great deal of social disorganization, distress, and alienation (Moos, 2006).
 The family system is greater than the sum of its parts. “The family” has meaning to its members separate from what each individual family member might mean. In other words, “family” is more than just a conglomeration of individual members living together. A family has an identity and “life” of its own. In many instances, family members act to further the family’s interests, even at individual expense. When an individual engaged in substance misuse violates this family-oriented expectation it is experienced as a gross violation by other family members. On the other hand, the possible impact on family is one potential protective factor stopping an individual from misusing substances—the impact on their family, not just on themselves. It also may be a motivating factor in someone wanting to engage in treatment and recovery—unfortunately, it can be difficult (as seen in the biological and psychological modules) to sustain this kind of family-focused motivation when substance use clouds a person’s mind and drives individuals’ substance seeking behavior.
The family system is greater than the sum of its parts. “The family” has meaning to its members separate from what each individual family member might mean. In other words, “family” is more than just a conglomeration of individual members living together. A family has an identity and “life” of its own. In many instances, family members act to further the family’s interests, even at individual expense. When an individual engaged in substance misuse violates this family-oriented expectation it is experienced as a gross violation by other family members. On the other hand, the possible impact on family is one potential protective factor stopping an individual from misusing substances—the impact on their family, not just on themselves. It also may be a motivating factor in someone wanting to engage in treatment and recovery—unfortunately, it can be difficult (as seen in the biological and psychological modules) to sustain this kind of family-focused motivation when substance use clouds a person’s mind and drives individuals’ substance seeking behavior. Family systems are comprised of subsystems. Family systems do not always operate as a whole; many interactions, roles, and functions are enacted within subsystems of the larger family system. These might include a couple subsystem, parent-child subsystems, or sibling subsystems. The possible variants are numerous especially when ex-partner, step-parent, step-/half-sibling, and extended family subsystems are involved. In families where a member is engaged in substance misuse, it is possible that the person’s “relationship” with the substances themselves functions much like a subsystem. For example, an adult son living with his mother—both of whom experienced active substance use disorders—described their two-person family in terms of there being “three of us” in the relationship—himself, her, and the drugs (quotingTony from the documentary entitled Foo Foo Dust).
Family systems are comprised of subsystems. Family systems do not always operate as a whole; many interactions, roles, and functions are enacted within subsystems of the larger family system. These might include a couple subsystem, parent-child subsystems, or sibling subsystems. The possible variants are numerous especially when ex-partner, step-parent, step-/half-sibling, and extended family subsystems are involved. In families where a member is engaged in substance misuse, it is possible that the person’s “relationship” with the substances themselves functions much like a subsystem. For example, an adult son living with his mother—both of whom experienced active substance use disorders—described their two-person family in terms of there being “three of us” in the relationship—himself, her, and the drugs (quotingTony from the documentary entitled Foo Foo Dust).- Change in any part of the system affects the entire system. Family systems are dynamic, changing over time as recognized in the chromosphere aspect of the social ecological model—past, present, and future look different because families are not static or stagnant. It is important to remember that all change—positive and negative in nature—are experienced as stressful, challenging the family system’s hard-earned balance and homeostasis. Consider, for example, how stressful happy family development events like marriage, childbirth, and retirement can be for the system; this adaptive pressure might bewilder families who only expected to be stressed by negative changes such as divorce or the death of a family member. Family system changes are a response to pressures from the outside (contexts), family membership, internal subsystems, and changes in individuals. Some pressures are developmental in nature—the dynamics of parenting young children may be very different from parenting adolescents, for example. It is the nature of systems that change in any part of the family system reverberates throughout the entire family system, sending ripples throughout the system.

Despite individual and family developmental changes presenting periods of stress, which in turn may trigger a transition from substance use to misuse or may trigger a relapse during recovery, it is also possible that family changes can lead to a reduction in substance use (Moose, 2006). For example, the transition to parenthood, while creating stress on the family system, also may lead young adults to adapt their substance use to become more aligned with role expectations of parents—certain adult roles are not compatible with alcohol and other substance misuse and therefore may exert pressure to reduce or cease substance use (Moos, 2006). Adolescents and emerging adults maturing and entering into important social roles often is associated with reduced substance use, perhaps due to greater responsibility and/or pressure from partners concerning what is no longer appropriate substance use; “maturing” out of substance misuse is less likely if misuse has progressed to the point of a substance use disorder (Begun, Bares, & Chartier, in press).
Role theory also has relevance for how a family member’s substance misuse might be experienced by the family system (Begun, Bares, & Chartier, in press). Family members adopt and fulfill roles that function to serve the demands of the social environment, the family as a whole, and the needs of individual family members (Begun, Hodge, & Early, 2017). While specific family roles, tasks, and behaviors vary by culture, context, time, and circumstances, key family functions include (1) obtaining and distributing resources necessary for meeting members’ basic needs for food, shelter, and protection, and (2) socialization of family members into family and societal roles (Begun, Bares, & Chartier, in press). Family dysfunction is common when one or more family member, particularly a parent, engages in substance misuse (Straussner & Fewell, in press). That individual’s expected roles could be:
- retained by, but poorly or inconsistently fulfilled by the individual engaged in substance misuse;
- delegated to other family members, potentially creating role overload situations for those individuals or role strain when the designated back-up player is ill-prepared for the role; or,
- unfulfilled, which in turn places the family system in a vulnerable state depending on how critical the role/functions are to the family and family members.
Recovery as Change Experienced by the Family System
 Outside of developmental changes, other individual changes can affect the family system as a whole: for example, a family member moving from substance misuse into recovery. Over time, a family may have adapted to the individual’s unpredictable, unreliable behavior while pursuing, using, and getting over the effects of using substances. Families may adapt to a member’s substance-related unpredictability and erratic functioning by excluding the individual from critical family roles (e.g., caregiving, financial decision making, intimacy). The family system exerts a great deal of energy and effort to achieve and preserve homeostasis under these rapidly shifting and unpredictable conditions. The family system again is challenged by the need to adapt to changes in the individual who engages in recovery efforts—how do family systems reintegrate these individuals and (again) provide them with meaningful roles? Despite recovery being a positive family event, all change in family systems is experienced as stressful—requiring the family to exert energy in (re)establishing balance. The system may not immediately respond in positive, accepting, welcoming, and trusting ways to the individual in early recovery, leaving that family member “on the outside looking in,” especially if they have been challenged to do so through multiple previous recovery efforts—they may be hesitant and not ready to place their trust in the recovery process. One member’s recovery can be especially challenging to couples when they have been engaged in substance misuse together; their relationship may have been built around their substance use. What may look like “sabotage” of the recovery process by family members may more realistically represent the family’s struggle to regain or retain homeostasis, even at the expense of or sacrificing one member’s well-being. For this reason, as well as to support individual family members affected by another member’s substance use, interventions at the couples and family system level are often recommended—helping the family to help itself as a whole and to support a member’s recovery efforts (McCrady, 2006; McCrady, Epstein, & Sell, 2003).
Outside of developmental changes, other individual changes can affect the family system as a whole: for example, a family member moving from substance misuse into recovery. Over time, a family may have adapted to the individual’s unpredictable, unreliable behavior while pursuing, using, and getting over the effects of using substances. Families may adapt to a member’s substance-related unpredictability and erratic functioning by excluding the individual from critical family roles (e.g., caregiving, financial decision making, intimacy). The family system exerts a great deal of energy and effort to achieve and preserve homeostasis under these rapidly shifting and unpredictable conditions. The family system again is challenged by the need to adapt to changes in the individual who engages in recovery efforts—how do family systems reintegrate these individuals and (again) provide them with meaningful roles? Despite recovery being a positive family event, all change in family systems is experienced as stressful—requiring the family to exert energy in (re)establishing balance. The system may not immediately respond in positive, accepting, welcoming, and trusting ways to the individual in early recovery, leaving that family member “on the outside looking in,” especially if they have been challenged to do so through multiple previous recovery efforts—they may be hesitant and not ready to place their trust in the recovery process. One member’s recovery can be especially challenging to couples when they have been engaged in substance misuse together; their relationship may have been built around their substance use. What may look like “sabotage” of the recovery process by family members may more realistically represent the family’s struggle to regain or retain homeostasis, even at the expense of or sacrificing one member’s well-being. For this reason, as well as to support individual family members affected by another member’s substance use, interventions at the couples and family system level are often recommended—helping the family to help itself as a whole and to support a member’s recovery efforts (McCrady, 2006; McCrady, Epstein, & Sell, 2003).

Positive Parenting
Evidence indicates that strong positive parent-child bonds, family involvement, sanctions against inappropriate behavior, (age appropriate) parental monitoring of their children’s behavior and experiences are protective, preventive factors in terms of substance use initiation and substance misuse (Moos, 2006). Parents establishing clear, unambiguous prohibitive norms concerning substance use/misuse, parental monitoring, and warm, positive relationships with their sons and daughters are protective factors against substance use/misuse. Reinforcing the importance of parents’ behavior is evidence concerning the preventive potential of parents’ own restraint in substance use, child monitoring, and substance-related norm setting (Carpenter, Dobkin, & Warman, 2016; Cook & Tauchen, 1984; Hawkins, Catalano, & Miller, 1992). The presence of positive father-child relationships was shown to decrease the probability of adolescent alcohol use, particularly within African American families (Jordan & Lewis, 2005).
Compensatory parenting. A considerable amount of clinical literature discusses the negative developmental outcomes and risks to children growing up in a family where one or both parents engage in substance misuse, potentially leaving children “functionally parentless” (Straussner & Fewell, in press). This is the case for about 87 million children aged 17 or younger: about 1 in 10 living in households where a parent experienced alcohol use disorder in the past year and about 1 in 35 in households where a parent experienced a past-year substance use disorder involving illicit substances (Lipari & Van Horn, 2017). Parental substance misuse clearly has the potential to impede parents’ ability to provide a safe and nurturing home for their children and raises the likelihood that children will be exposed to an array of environmental stressors (Straussner & Fewell, in press).
It is important also to consider the problem from a strengths-perspective, however: assessing the protective and resilience-promoting factors that may be operating in the child’s environment, too (Begun & Zweben, 1990). One concept to consider is the possibility that parenting deficits are being otherwise satisfied by significant others in the child’s life—children with the ability to elicit this type of compensatory parenting may be more resilient than others living under the same challenging conditions. For instance, children of parents with alcohol use disorder who elicited positive caregiver experiences from other caring adults showed a reduced probability of poor coping outcomes compared to other “less resilient” children in similar circumstances (Werner, & Johnson, 2004).

In short, it might be helpful to consider how the functions of parenting and caregiving are met when looking at children’s experiences of the social and physical environment, rather than focusing only on the persons who are parents. Positive, stable compensatory relationships represent potentially significant contributions to a child’s or adolescent’s resilience (Begun, Bares, & Chartier, in press). Compensatory parenting is often provided by grandparents (see Mendoza, Fruhauf, & Hayslip, in press), other extended family members, other social contexts (e.g., school personnel or peers’ family members; Werner & Johnson, 2004), or through formal foster care arrangements.
Family Disease Model
Earlier modules discussed debates concerning the disease model of addiction. Here we consider the family disease model of addiction. This perspective stems from an awareness of how one family member’s substance-related problems affect other family members—especially in couples’ and parent-child relationships (McCrady, Epstein, & Sell, 2003). The whole family might be viewed as suffering from the disease of addiction. As a family disease, this might be characterized by family role, communication, and relationship dysfunctions that perpetuate (enable) the individual family member’s addictive behavior. The implication is that treating addiction requires intervention with families, not just individuals. In family systems terms, the individual clearly affects the rest of the family and the family clearly affects the individual.
However, the family disease model becomes controversial when relying on a definition of the family disease as codependency. The codependency assumption is based on observations that certain traits and characteristics commonly occur within families experiencing a member’s addiction. The defining traits involve family members’ behaviors being organized around the one member’s addiction-related behaviors. In codependency, family members’ behaviors are viewed as supporting or enabling the dysfunctional behavior of the person experiencing addiction because they have come to depend on that person’s dysfunctional behavior being maintained. The logical extension that has been inferred involves allowing the person’s life to completely fall apart (“hitting rock bottom” or, at least “high bottom”) and withholding love (or delivering “tough love”) as means of motivating the person to change (Szalavitz, 2016). The evidence supporting this contention is weak and inconsistent, at best; evidence suggests that it actually inflicts additional psychological harm and many family members refused to engage in this manner without being part of a dysfunctional family system (Szalavitz, 2016).
The codependency model has become highly controversial, with many practitioners and researchers arguing against applying the label or diagnosis of codependence. First, many behaviors identified as codependent can be viewed as reasonable adaptive responses rather than causes (or enabling) of the family member’s addictive behavior. For example, compensatory parenting, while it may remove some negative consequences of a parent’s substance-related neglect of their child’s caregiving needs is important as a means of ensuring the child is protected and nurtured in important ways—thus, it is adaptive for the child rather than maladaptive for the parent, enabling the substance misuse to continue. Second, many of the observed behaviors also occur in healthy families, or at least in families where no member experiences addiction; the behaviors not being unique to families where a member experiences addiction means they are not diagnostic of a family disease process. Third, the label “codependent” has become overused, imprecise, and “blames” or “shames” family members for the problems they experience as a family. Finally, while “clinical descriptions of codependency are common, empirical support for the concept is lacking…there are no compelling empirical data to support the full construct of codependency” (McCrady, Epstein, & Sell, 2003, p. 120). Despite this level of controversy, the family disease model confounded with codependency constructs continues to underlie some intervention approaches.

Supportive Significant Others
Family members and others in a person’s social context may play a significant role in recovery (Begun, Bares, & Chartier, in press); recovery is a process heavily influenced by social processes and occurs within social contexts (Heather et al., 2018). Individuals in recovery from an alcohol or other substance use disorder engages in frequent, proximal, microsystem interactions—these might be with family, friends, co-workers, and members of mutual/peer support groups (Begun, Bares, & Chartier, in press). These individuals are considered significant others (SOs) in the person’s physical and social recovery contexts. Different SOs, at different times, and through different behaviors may support the individual’s recovery efforts, complicate the efforts, or be irrelevant to the recovery efforts. When they are acting in support of recovery, they can be identified as supportive significant others (SSOs). Intervention with SOs might involve training them to be supportive of recovery, to be effective as SSOs. Mutual/peer help programs (e.g., 12-step programs and other recovery support organizations) offer a person in recovery a network of SSOs, as well as creating opportunities for supportive physical environments (e.g., sober housing and social events). A focus of the twelve-step facilitation intervention is to help prepare individuals to effectively engage with and benefit from participation in mutual/peer support programs available in their communities.
A controversial aspect of family members and friends supporting a person’s recovery is represented in the television show Intervention. The show demonstrates the implementation of the Johnson Intervention confrontational approach for motivating a person’s entry into treatment for a substance use disorder. Members of the person’s social network confront the individual about the damage caused by their substance misuse and offer an ultimatum concerning the actions they will take if treatment is not engaged (Loneck, Garrett, & Banks, 1996). A critical review of the television show raises concerns about this use of the SOs (Kosovski & Smith, 2011). These include:
- footage is heavily edited to appeal to a (distorted) reality-television-consuming audience;
- the populations depicted poorly reflect the diversity of individuals engaged in substance misuse or experiencing substance use disorders;
- the treatment options, availability, and accessibility represented are a glaring misrepresentation of what treatments are available, affordable, preferred, and successful;
- data provided by the show concerning the success rate of the interventions in helping individuals enter and complete treatment are misleading and grossly misrepresent the intervention outcomes.
These authors cite literature indicating that fewer than 30% of families encouraged to engage in the confrontational intervention method actually follow through and host such an event, and that a relatively small percentage of individuals enter into additional treatment following such an intervention (Kosovski & Smith, 2011). They concluded that other family-based models used to engage individuals in treatment are more effective and have been evaluated with greater rigor than the Johnson Intervention model. In other words, this approach does not represent a positive, effective role for SOs to act as SSOs.

Construct an eco-map of your own social contexts.
Identify the relationships you have with your social environment that might “push” toward substance use/misuse.
Identify the relationships you have with your social environment that help resist substance use/misuse.
Think about how this picture might have changed over time and could change in the future.
Consider what you learned from your own eco-map that can help you understand the eco-map of a person experiencing problems with alcohol, tobacco, or other substances.
