Chapter 14: The Eye
Fibrous Tunic
The fibrous tunic is comprised of 2 components, the clear cornea and the opaque sclera. They differ primarily in the arrangement or organization of their collagen and water content with this accounting for the difference in their transparency.
Cornea
The mammalian cornea is a transparent, avascular structure that functions to transmit and refract light, and as a protective barrier for the internal ocular contents. Although the cornea is avascular, it does contain nerve fibers. These are branches of the ophthalmic branch of cranial nerve 5 and are primarily concentrated in the anterior third of the cornea.
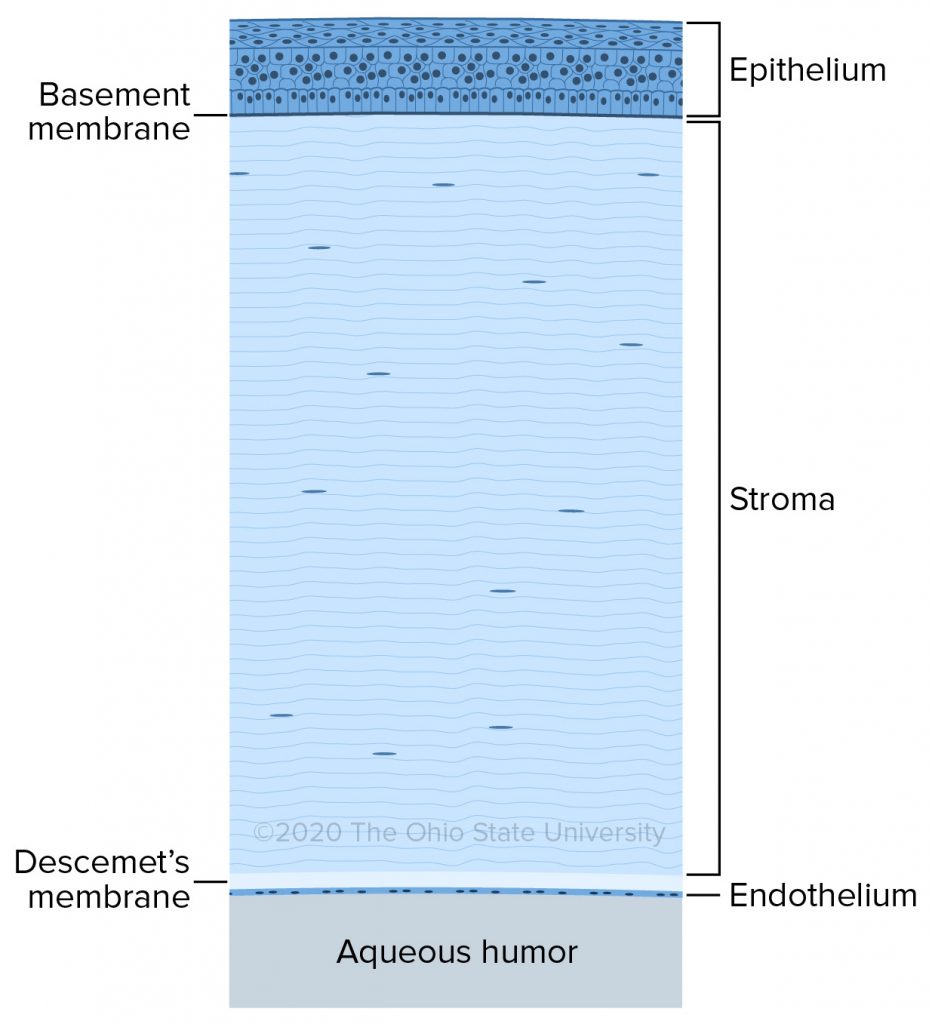
In general, the cornea of various species is remarkably similar, differing in thickness, curvature, and shape only. The cornea is thickest peripherally. The histologic layers of the cornea, from the outside in, are the corneal epithelium, the corneal stroma, Descemet’s membrane and corneal endothelium.
Corneal Epithelium
The corneal epithelium is composed of a stratified squamous, non-keratinized cell layer. Embryologically, the cells of the epithelium originate from surface ectoderm. The number of epithelial cell layers varies in thickness with the species and increases in number towards the limbus. Epithelial cells are anchored to each other by desmosomes and to the basement membrane by hemidesmosomes and anchoring fibrils. External to the epithelium is the tear film. The tear film supplies oxygen to the cornea and approximately 10% of the glucose used by the cornea. The epithelial cells are divided into basal, wing, and superficial cells. The superficial cells have microvilli, microplicae, and a glycocalyx on their surface to stabilize the tear film. Beneath the superficial cells are the wing cells that represent a transition zone between the basal and superficial cells. A single layer of tall, columnar basal cells is the deepest layer of the epithelium. These cells contain abundant glycogen stores and are the source of cells for the renewal of the outer layers. The turnover rate of these cells is 7 days. In addition to the outer layers of the epithelium, the basal cell layer is also responsible for the secretion of the basement membrane. This membrane is composed of type IV collagen and glycosaminoglycans (GAG’s).
Stroma
The corneal stroma comprises 90% of the corneal thickness. It is composed of collagen fibers, keratocytes, and GAGs that account for 22% of the stroma. The remaining 78% of the stroma is water. The collagen fibers are regularly arranged in lamellar sheets and span the entire diameter of the cornea. These lamellae lie parallel to the corneal surface, but obliquely to adjacent lamellae. The transparency of the cornea depends on the arrangement of these lamellae and the distance between them. It is hypothesized that an interfiber distance of less than a wavelength of light allows transmission with minimal interference. The normal collagen in the corneal stroma is type I and is more heavily glycosylated than in skin. When injured this is replaced by type III collagen. Between the corneal collagen fibers are flat cells termed keratocytes and GAGs. The keratocytes are capable of fibroblast transformation and phagocytosis, but normally are a quiescent population of cells. The GAGs of the stroma affect hydration, thickness, and transparency. Lymphocytes and Langerhans cells are also reported in the cornea, especially near the limbus.
Descemet’s membrane
The posterior limiting membrane or Descemet’s membrane is a basal lamina secreted by the endothelium . It is comprised of type IV collagen and is produced throughout life, continuing to increase in thickness with age. It is insoluble except in strong acid or alkali and is more resistant to collagenase than is the corneal stroma.
Endothelium
The innermost layer of the cornea is the endothelium. The origin of this layer is thought to be the neural crest cells. The endothelium is a single cell layer of hexagonal cells, 15-20 um in diameter, attached to each other by terminal bars. In most species these cells are capable of mitosis only very early in life. The greatest cell density of the endothelial cells is in the neonate. Once damaged, endothelial cells repair defects through enlargement and spreading rather than by replacement.
Sclera
The sclera constitutes the major portion of the fibrous tunic and joins the cornea at the limbus. Anteriorly it is covered by bulbar conjunctiva beneath which is the episclera, the scleral stroma, and the lamina fusca. The episclera is composed of loose bundles of collagen and elastic fibers, blood vessels, nerves, fibroblasts and, depending on the species and color pattern, melanocytes. Like the corneal stroma that of the sclera consists of collagen lamellae but unlike the cornea they are obliquely arranged and lack uniformity. This lack of uniformity, along with the variability in collagen fiber diameter and the relative deficiency in water-binding glycosaminoglycans’s, account for the lack of transparency to the sclera. The sclera possesses several channels or emissaria to allow the passage of nerves and blood vessels. Examples of these are the optic nerve, the vortex veins, long posterior ciliary arteries, and the long and short ciliary nerves. These emissaria are weak points and are potential sites of rupture following a trauma.
